Beginner's Guide to SleepyHead
RobySue's Beginner's Guide to SleepyHead was originally posted on the Apnea Board Forum. Her original posts were lost during a database update. This wiki article was created from a cache of her posts and has been updated by Sleeprider.
_________________________________
Please Note: SleepyHead is no longer maintained. It has been replaced by the OSCAR software package, available at:
https://www.SleepFiles.com/OSCAR
_________________________________
Questions concerning the SleepyHead software may be posted in Apnea Board's Software Support forum. You may register for a free forum account here.
Contents
- 1 Installing SleepyHead
- 2 Running SleepyHead for the first time
- 3 Basic SleepyHead Organization
- 4 Basic data interpretation: Daily Detailed Data
- 4.1 Left Side Bar data---AHI and event data table
- 4.2 Left Sidebar Data---Statistical Data chart
- 4.3 Important Daily Detailed Graphs
- 4.4 The Event Table---a detailed look
- 4.5 The Flow Rate graph---a detailed look
- 4.6 The Pressure graph---a detailed look
- 4.7 The Leak Rate graph---a detailed look
- 4.8 The AHI Graph
- 5 Basic data interpretation: Overview Data
- 6 Basic data interpretation: Statistics Data
- 7 Important preferences settings
- 8 Leaks
- 8.1 Difference between Total Leak Rate and Leak Rate
- 8.2 Definition of Large Leak
- 8.3 Perfect Leak/Total Lines
- 8.4 Good and Decent Enough Leak/Total Leak lines
- 8.5 Problematic, Bad, and Horrible Leak Lines
- 8.6 Mouth Breathing and Other Causes of Leaks
- 8.7 Annoying Leaks
- 8.8 Why are Large Leaks an Issue?
- 9 Beyond AHI: Apneas and hypopneas in the Flow Rate graph
- 9.1 Flow Rate graph: A trace of every breath you took
- 9.2 Basic scoring criteria for apneas and hypopneas
- 9.3 Obstructive and central apneas
- 9.4 Other flagged events
- 9.5 RERAs
- 9.6 Periodic Breathing
- 9.7 Wake breathing and "False" events (Sleep-Wake-Junk)
- 9.8 Sleep transition breathing and "False" events
- 9.9 Lengths of individual events
- 9.10 Clusters of events
- 9.11 How APAP machines respond to events
- 9.12 Snoring Data
- 9.13 Flow Limitations
- 10 Fancy Stuff: Other Data Available from SleepyHead
- 11 Manipulating Daily and Overview Graphs
- 12 Posting SleepyHead Graphs to the Forum
- 13 Tricks and Shortcuts
- 14 SleepyHead FAQ
- 14.1 Q: Can SleepyHead change or erase the data on my SD card?
- 14.2 Q: I imported my data into SleepyHead and when I put the card back into my ResMed S9, I get an error that says: " 'Invalid SD card, erase card data?". Why is this happening and what should I do?
- 14.3 Q: Will SleepyHead work on my computer?
- 14.4 Q: My computer doesn't have an SD card slot. Can I still use SleepyHead?
- 14.5 Q: Is there a list of keyboard short cuts and mouse tricks for SleepyHead?
- 14.6 Q: I forgot to put my SD card back into my CPAP after importing the data into SleepyHead. Have I lost my data?
- 14.7 Q: How often do I need to import my data into SleepyHead?
- 14.8 Q: I've downloaded my data from a ResMed S9 Elite, AutoSet, VPAP S, or VPAP Auto, and there is no detailed data and SleepyHead says I didn't use the machine. What did SleepyHead do with my data?
- 14.9 Q: I don't see any Flow Rate data. What am I doing wrong?
- 14.10 Q: Can SleepyHead work with data from an oximeter?
- 14.11 Q: Can SleepyHead tell me when I was in REM sleep?
- 14.12 Q: Can SleepyHead tell me when I was awake during the night?
- 14.13 Q: Can SleepyHead tell me when I was sleeping on my back?
- 14.14 Q: I'd like to post some SleepyHead data to the forum, what should I do?
- 14.15 Q: Where can I report bugs?
Installing SleepyHead
System Requirements
To use SleepyHead to analyze your data you need an xPAP that can store data on a Secure Digital (SD) memory card and an appropriate SD card in it, and a personal computer running Linux, macOS, or Windows. At this time the program is not supported on tablets or mobile devices.
While many DMEs include an SD card when they set up an xPAP, some DMEs do not; it is important to verify your xPAP has an SD card installed.
Note: Sleepyhead does not support tablets or mobile devices.
Machines Supported by Sleepyhead 1.1.0 and OSCAR 1.1.0:
See the article (OSCAR_supported_machines)
Step 1. Download SleepyHead
As of January 2019, the last version of SleepyHead for Macintosh, Windows and Ubuntu Linux was SleepyHead 1.1.0. SleepyHead is no longer maintained and has been replaced by the OSCAR software program.
Step 2. Installing SleepyHead
For Windows:
SleepyHead 1.1.0 runs on Windows XP, Vista, 7, 8, and 10. Download the Windows install file, run it and follow the instructions. Depending on your security settings, you may be required to enter Administrator credentials.
The install program will put a SleepyHead (sheep) icon on the Start Menu. If you want a short cut installed on the desktop or task bar, create those short cuts the same way you do for any other Windows program.
The installer places both the OpenGL and BrokenGL versions in Program Files and lists them in the Start Menu. These versions will be explained below.
Before placing any shortcuts on your desktop it is best to launch OpenGL, which is the preferred version. If it works for you, then create a shortcut for OpenGL on your Desktop or Taskbar (or both). Otherwise launch the BrokenGL version from the Windows Start Menu and verify that it works before placing shortcuts where you like.
Program Location and Broken-GL in Windows
Sleepyhead installs by default into Windows in the C:\Program Files(x86)\Sleepyhead. At the bottom of the list of folders and files are two EXE files:
- Sleepyhead.exe
- Sleepyhead-BrokenGL.exe
Some computers do not have a video card that meets the Open-GL video Graphics standards. If you have problems with displaying Sleepyhead, or it does not run when clicking on the Sleepyhead.exe link, use the Sleepyhead-BrokenGL.exe. This version solves most installation problems.
Default Data File and Screenshot Locations in Windows
The default file location for the Sleepyhead data is in C:Users\{username}\Documents\Sleepyhead This is be shortened in some computers to My Documents\Sleepyhead.
Profiles Sleepyhead can have multiple profiles for a user. The profiles are stored in My Documents\Sleepyhead\Profiles\{username}.
Machines Each SleepyHead user's profile must have one and can have several machines, each having a unique identifier. SleepyHead creates folders for each machine for Backups, Events and Summaries. This information may be backed up and can be transferred to any new installation of Sleepyhead.
Screenshot Image Files When you take a screenshot in Sleepyhead using the F12 key, it will be saved in the Screenshots subfolder. Screenshots are stored in full size and resolution using the Portable Network Graphic (.PNG) file type.
For Macintosh OS X:
SleepyHead 1.1.0 runs on Macs running OS 10.7+. The downloaded SleepyHead-1.1.0 dmg file should open up as a "Volume." Simply drag the SleepyHead icon to the Applications folder. Once the SleepyHead application has been copied to the Applications folder, it's useful to drag it to the Dock so that launching SleepyHead is easy.
The downloaded SleepyHead-Testing-0.9.8-1-T3-MacOSX.dmg or SleepyHead-Testing-0.9.8-1-T3-MacOSX-BrokenGL.dmg should open up as a "Volume" and you simply drag the SleepyHead icon to your Applications folder. Once the application has been copied to the Applications folder, it's useful to drag it to the Dock so that launching SleepyHead is easy. The "OpenGL" version will work with high performance video systems while the "BrokenGL" should work with all Macs. If in doubt, choose the BrokenGL version.
For Linux:
SleepyHead 1.1.0 has an automated installer for Unbuntu 15.04. Download the installer, run it and follow the instructions. There is no installer for any other version of Linux. However, experienced Linux users can download the source and compile it if they want to run SleepyHead on a Linux system other than Unbuntu 15.04. Source code for SleepyHead is found in this Sourcecode folder.
There are several different Linux packages available. Some older versions are stored in the Releases folder on the Sourceforge site. You can find them by going here. Select the appropriate package for your particular Linux machine. Install the software in the normal way for your system. NOTE: I have NOT installed SleepyHead on a Linux system, and I don't know how well the packages work. Most Linux users know their way around their system however, and are not newbies when it comes to downloading software. For the newer versions of SleepyHead for Linux, please refer to the wiki instructions on Building SleepyHead from Source and a forum thread here.
Reinstalling Sleepyhead and Attaching Existing Data
Place-holder for article extension http://www.apneaboard.com/forums/Thread-SH-1-won-t-see-SH-9-data?pid=249253#pid249253
High Resolution Monitors
If you use an ultra high definition monitor (UHD), the print size may appear extremely small or be unreadable. To resolve this problem:
- Go to whatever folder containing the Sleepyhead.exe program.
- Right click on 'SleepyHead.exe'.
- Left click on 'Properties'.
- Left click the 'Compatibility tab'.
- Left click box for 'Overide high DPI scaling behavior'.
- Scaling performed by: Click on drop down box just below and select 'System'.
- Click Apply, then Okay.
Additional Notes
SleepyHead works on Macs running most modern OSX systems without any problems. On Windows machines, SleepyHead 1.1.0 should install cleanly on anything from XP through Windows 10. If you run into problems with installing on Mac, Windows or Linux, please post your question in the Software Support Forum and someone will likely be along soon to help.
Running SleepyHead for the first time
First time users of SleepyHead are sometimes confused about what they have to do when they open up SleepyHead for the very first time.
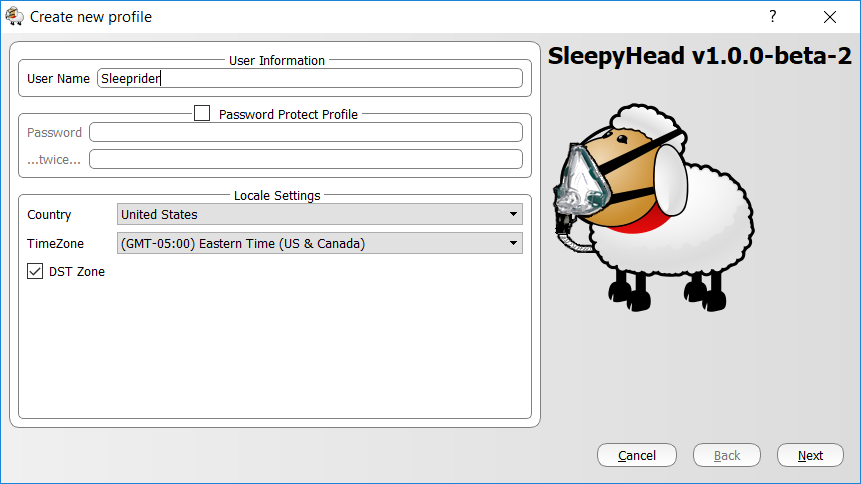
Creating a Profile
When you first open up SleepyHead, you will be asked to create a profile. The process is pretty straight forward, but you do have to do it before you can use SleepyHead to download your data. The first page of the Profile builder looks like this:
If you are using a Philips Respironics machine, the most important part of the profile is to make sure you get the time zone correct on this first page. SleepyHead uses the time zone information to take the timestamps on the data and adjust it to local time if your machine uses GMT when recording the data. It's also important to remember to check the Daylight Savings time box if appropriate. If you make a mistake, you can edit the profile later. But it is easier to get the time right when you are creating the profile.
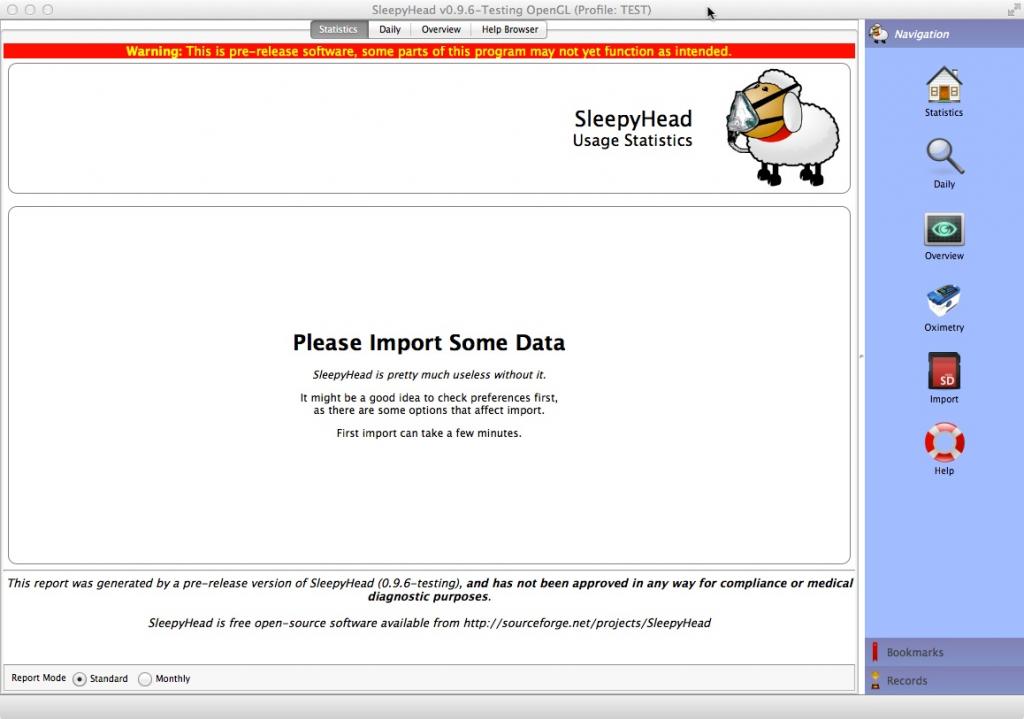
Once the profile is finished and saved, SleepyHead will display a blank page that looks like this:
As the page says, it's reasonable to click on Preferences and double check some things first. If you need help, jump to 7. Important preference settings
The main point here is that if you start clicking around looking for your data, it won't be there. You still have to download (or import) the data into SleepyHead.
Importing Data into SleepyHead the FIRST time
Put the SD card into the SD slot if you have not already done that. If your computer does not have an SD slot, you will need to buy a generic SD card reader and put the SD card in that.
WARNING: It's wise to make sure the card is locked if you are using a Mac or a Windows 8.1 or Windows 10 machine since these operating systems will write hidden files to unlocked cards. And the ResMed S9 machines will reject SD cards with any extra files written on them. See Secure Digital (SD) memory cardfor instructions on locking a card.
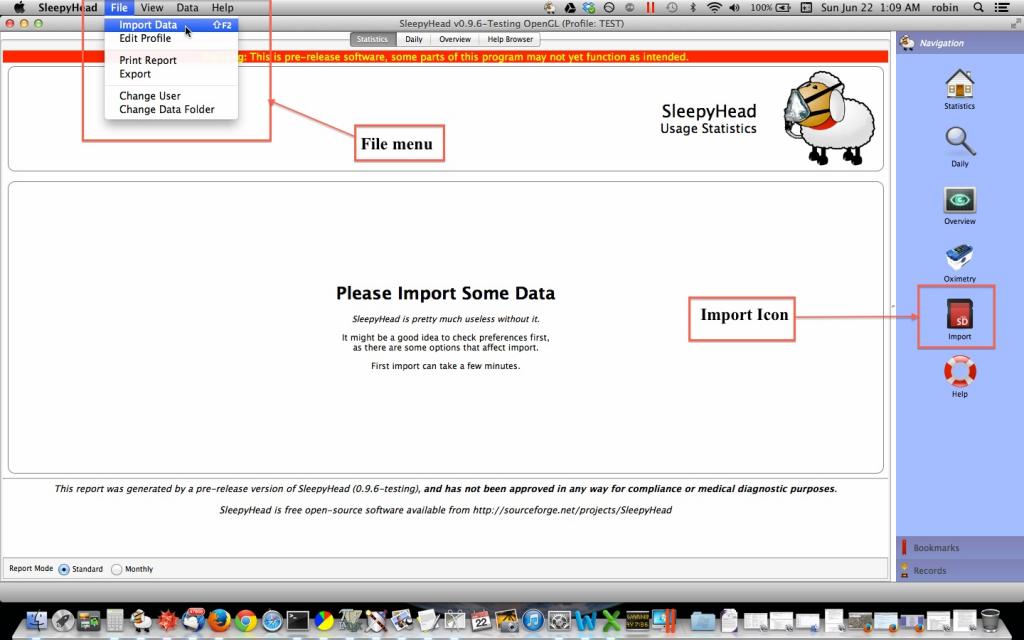
Once the card has been mounted to the computer system, you still need to import the data into SleepyHead. There are three different ways to Import the data:
- The Import Icon on the sidebar. Click this and it starts the import process.
- The Import Data under the File sub-menu. Select this from the standard File menu in the usual way for your system and it starts the import process.
- The keyboard shortcut. On a Windows machine you can simply press the F2 key and that will start the import process.
The Import Data menu item and the Import Icon are circled in the screen shot below.
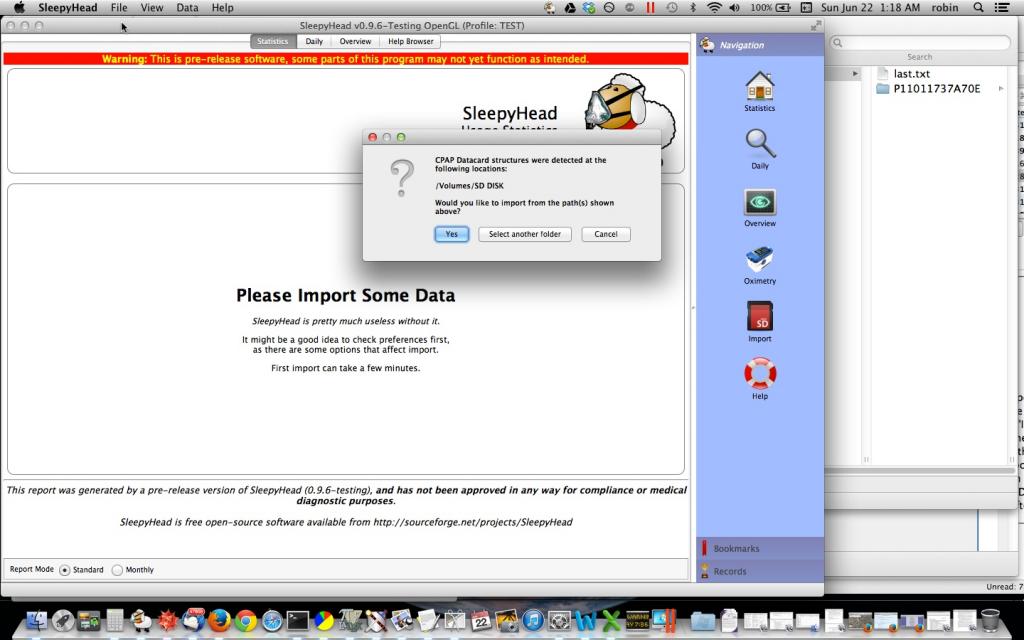
With your SD card is in the SD slot or card reader, once you click on Import Data, you will get a small pop up dialog box that looks this:
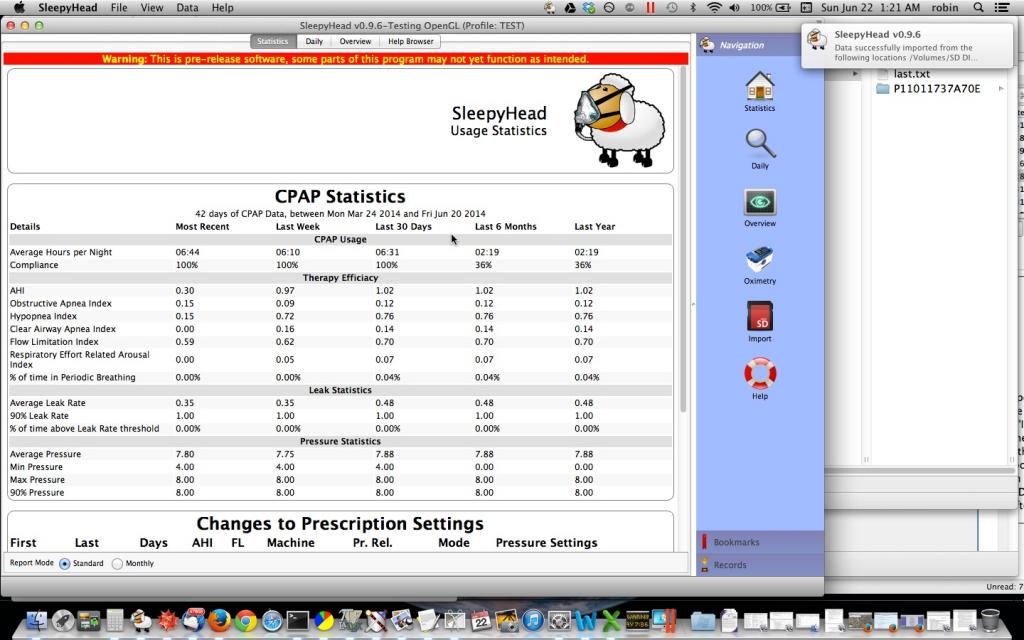
Click "Yes", and the data should load. After the initial data import, SleepyHead should display your data in a screen that shows the Statistical Data. It looks like this:
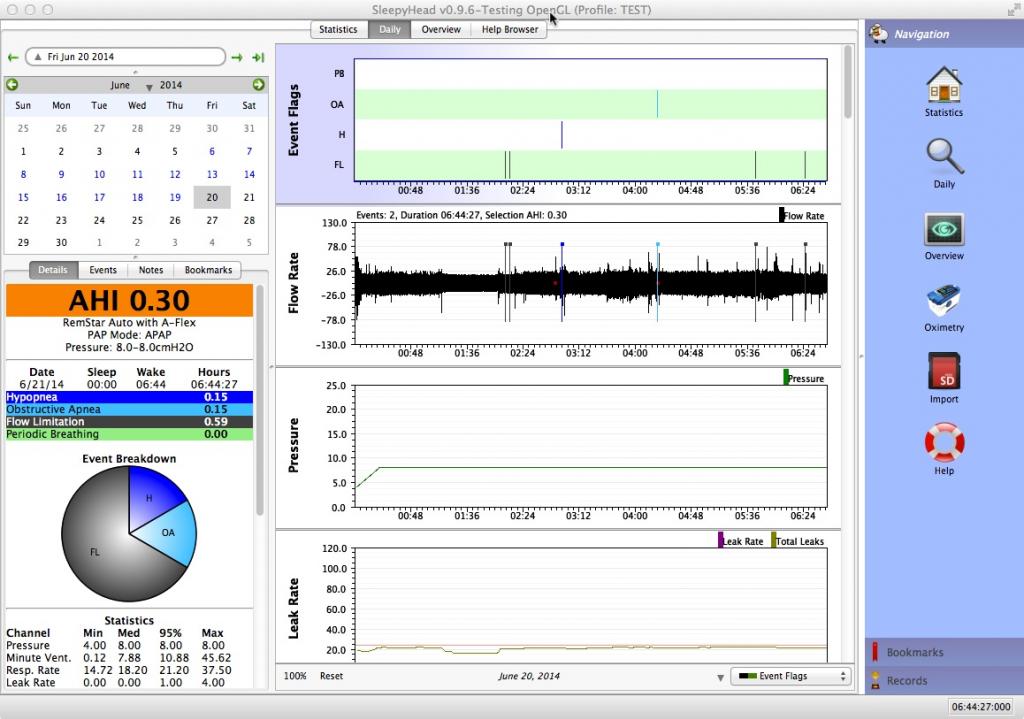
Clicking on the Daily tab in the SleepyHead window brings up the Detailed Daily Data for the last day of data:
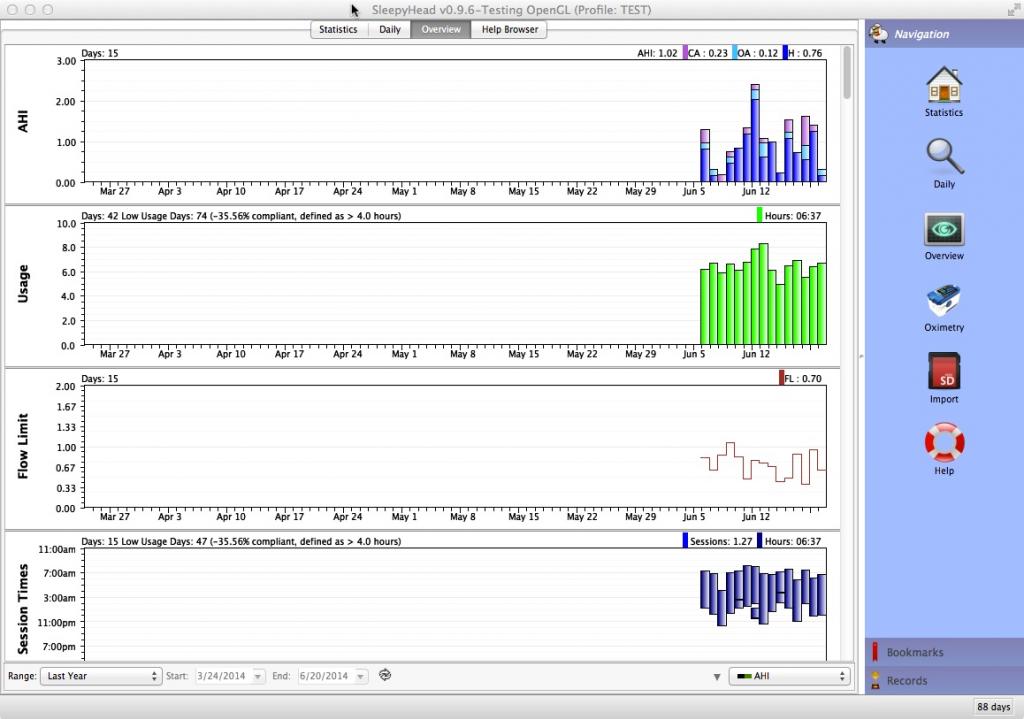
Clicking on the Overview tab in the SleepyHead window brings up the bar graph data for the last year of data:
Image has been scaled down 25% (777x546). Click this bar to view original image (1024x719). Click image to open in new window.
NOTE: The images used were from a data card that had limited data on it, so that's why all the overview data is at the far right of the screen: The import didn't include any detailed data that was older than June 6, 2014.
Importing Data into SleepyHead AFTER the first time
Each time you want to import data into SleepyHead you go through the same basic process, except you don't have to create the profile:
Step 1. Open SleepyHead
SleepyHead will bring up a list of profiles for you to chose from. For most people, there will only be one name on the profile. Highlight the desired profile and press the Select User button. The data for that profile will load into SleepyHead and the Statistics page should load.
Step 2. Make sure the SD card is in the SD slot or card reader.
It's wise to make sure the card is locked if you are using a Mac or a Windows 8.1 machine since these operating systems will write hidden files to unlocked cards. And the ResMed S9 machines will reject SD cards with any extra files written on them.
You will need to have the card in the Write Enabled (unlocked) condition while it is in the S9 and Write Protected (locked) prior to inserting it into your computer. Also, some of the newer low cost card readers do not have the micro switch installed in the unit. This means that even if you have it write-protected, it may not stop it from having the system files written by the PC.
To be safe you may wish to download and use the following script. It will turn off(or back on) this feature on your PC. Prevent SysVol Info Write
Step 3. Import the Data
Once SleepyHead loads the data for the selected Profile and the SD card is mounted, you can import the (new) data by either pressing the Import icon, using the File menu to select Import Data, or the keyboard shortcut---pressing the F2 key. The Import dialog box will appear and if you are importing from the After the first data importation, you can import the data regardless of which data view you are looking at. If you import data while in the Daily Data view, the Daily Data will jump to the last day of imported data after the data is successfully imported.
Additional Notes
1) The process for importing the data is easy once you get used to it.
2) Remember to properly unmount the SD card from your computer before removing it from the SD slot or card reader. You unmount the SD card the same way you unmount a flash drive or an SD card from a digital camera.
3) Remember to put the card back into your CPAP machine. This is particularly true for ResMed users: All the detailed data is written directly to the SD card, and if there is no SD card, that data is lost. And SleepyHead will report that there is no data for the night. (ResScan will be able to report on the summary data that is stored in the S9's memory and then written to the card when it is inserted into the machine).
Basic SleepyHead Organization
When first learning how to use SleepyHead, it helps to have a basic understanding of the organization of each of the data views are available in SleepyHead.
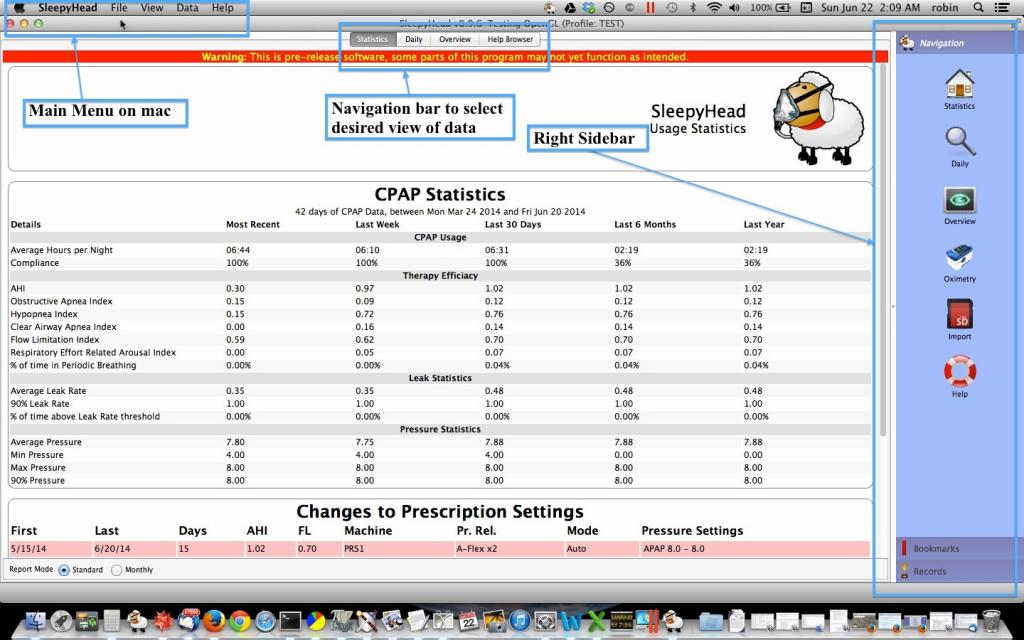
Basic Parts of the SleepyHead Window in All Views
When you start SleepyHead and select the profile you wish to use, SleepyHead opens up the Statistics page, which is as good of a place to start as anywhere else for looking at the overall organization. Here's a marked up copy of what you see on a Mac:
The Main Menu on Windows is at the top of the SleepyHead window (like the Main Menu for any other application). It's a pretty standard main menu and is the same in both Windows and Mac versions.
The Navigation Bar is always visible and it's always in the middle of the top part of the window on a Mac, and below the Main Menu on the left in Windows. Clicking each button on this Navigation changes the data. Each of the data views will be examined in more detail further down in this article.
The Right Sidebar duplicates the Navigation bar AND adds an Import icon that can be used to start the import data process talked about in 2. Running SleepyHead for the first time. The Right Sidebar usually takes up a lot of real estate on a laptop computer. You can turn the Right Sidebar off by pressing the F8 button on the keyboard. (On a Mac you may have to use Shift-F8 depending on how you have your function keys set up.)
===The Main Menu---a closer look===
The Main Menu has four submenus:
- File
- View
- Data
- Help
On the Mac, the SleepyHead menu is a standard "Application" menu with the standard things, including "Preferences" and "Quit SleepyHead". Windows applications don't have this "Application" menu.
===The File menu===
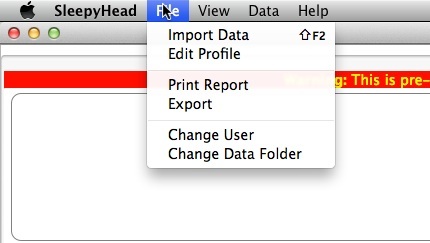
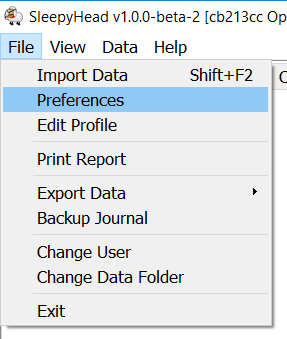
The File menu looks like this on a Mac:
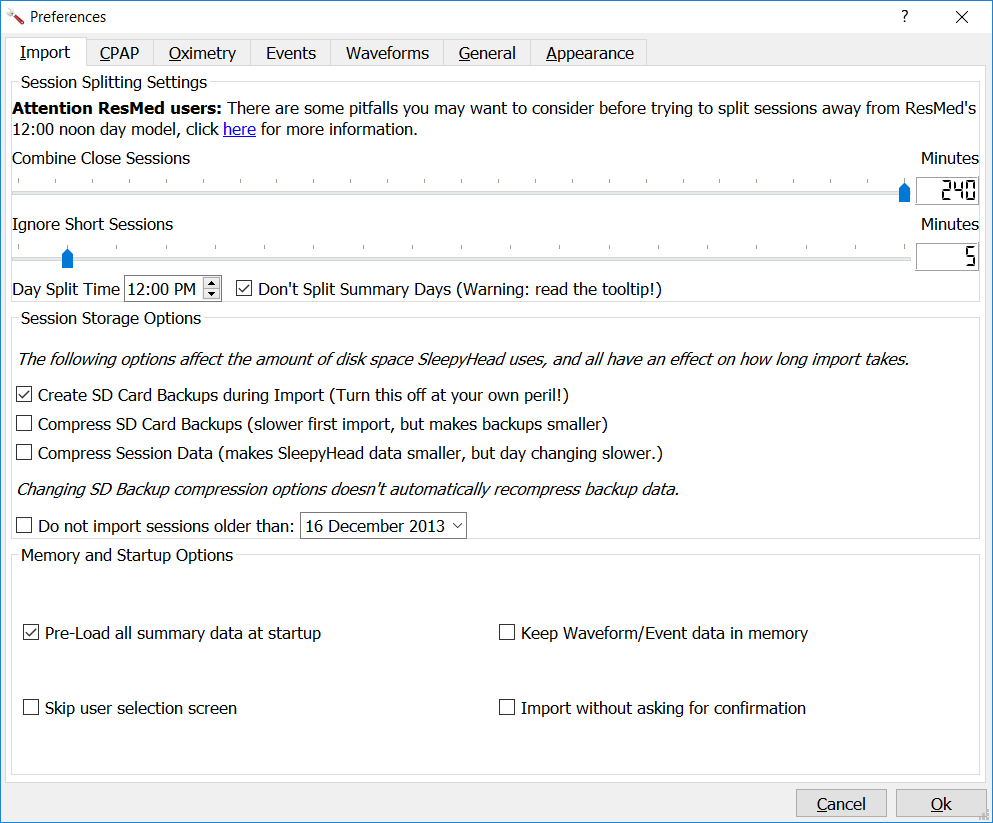
In Windows, the File menu looks much the same except that it also contains "Preferences" and "Exit" as menu options. The Preferences Menu is particularly important as it opens menu choices to adjust settings for Import, CPAP, Oximetry, Events, Waveforms and Appearance. See SleepyHead Chart Organization to see how these Preferences are used in organizing your charts. (Preferences are under the SleepyHead menu on the Mac).
For a new SleepyHead user, the most important options on this menu are the "Import Data" and "Edit Profile". In Windows, add "Preferences" to that list. For now you can ignore the other options under the File menu.
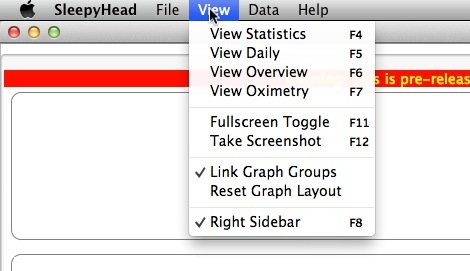
The View menu looks like this on both a Mac and a Windows machine:
It's important to keep "Link Graph Groups" checked (Mac only). As long as that's checked, when you zoom in on one of the daily graphs, all the daily graphs will zoom in the same amount. That's very useful when you need to look at more than one graph to see what's going on.
Unchecking "Right Sidebar (F8)" will make the Right Sidebar disappear, which gives the graphs in the Daily View more room.
"Fullscreen Toggle (F11)" Prepares the Sleepyhead screen for a screenshot by hiding personal identifying information and closing the right sidebar. Remember if you toggle to full-screen using F11, you must toggle back using F11 again to see the menu controls.
"Take Screenshot (F12)" is also self explanatory. In earlier versions of SleepyHead, this was really buggy. It seems to work much better in SleepyHead 0.9.5 and 0.9.6. On a Mac, SleepyHead will tell you the location of the saved screenshot. On a very small netbooks running Windows 7, it's not completely clear whether "Take Screenshot" works and it does NOT tell the user the location of the saved screenshot.
The Data menu looks like this on a Mac:
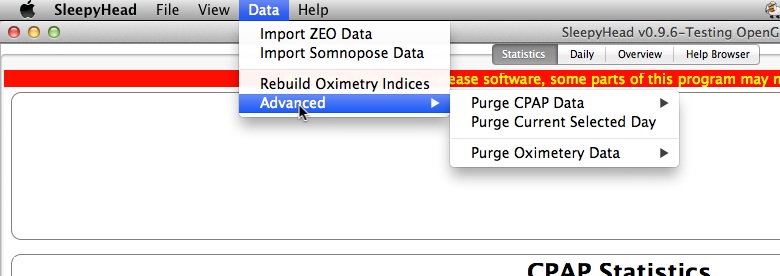
The Windows menu is very similar, but has a few differences. For a new user of SleepyHead, the only item on this menu that you may need is the Purge CPAP data options under the Advanced menu item. When Zeo was still in business, a lot of us were using Zeos as well as CPAPs. And Import Zeo data was (and remains) a way to get Zeo data into SleepyHead. It does require doing some things within the Zeo itself to make the import run smoothly.
If you plan on using SleepyHead with an oximeter, please see Importing CMS 50D Plus oximeter data into SleepyHead, this forum thread, or or post your questions on the Software Support Forum.
Parts of the Daily data window
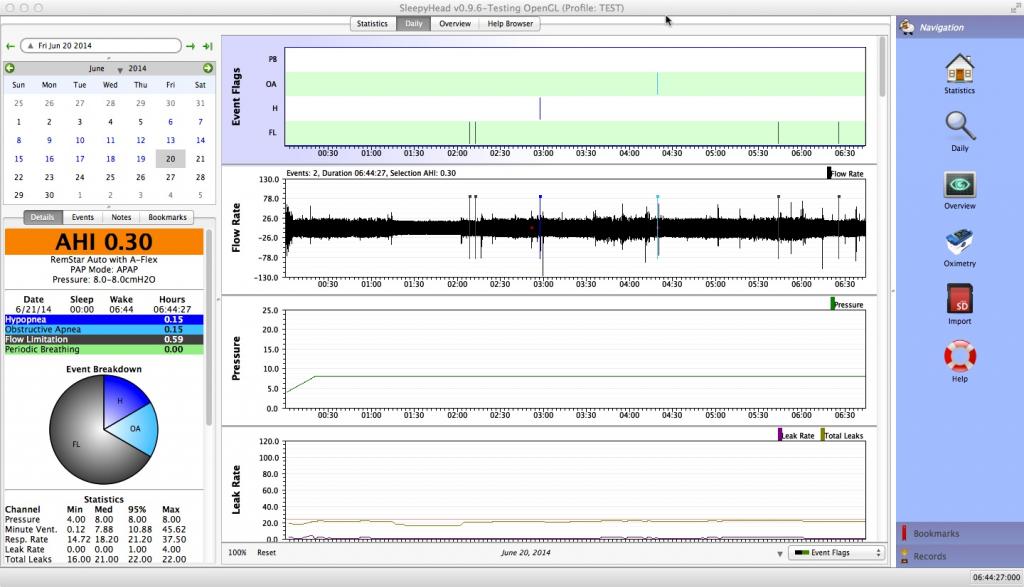
The format of the Statistics and Overview pages is straightforward. But it's worth looking at the pieces of the Daily Data window as part of the basic organization in SleepyHead. Here's a typical Daily data window for a Philips Respironics System One Auto:
The window has four major parts:
- The calendar in the upper left corner
- The Left side bar below the calendar with numerical data
- The detailed daily graphs in the middle of the window
- The Right Sidebar, which can be turned off in order to give the graphs more horizontal room.
We'll look at each of these parts except for the Right Sidebar in a bit more detail.
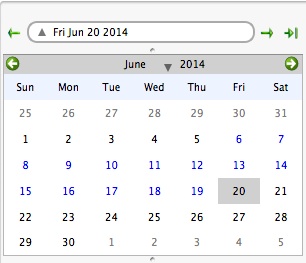
The Calendar
The calendar allows you to both identify what day's data you're looking at:
The calendar can be useful for navigation, but if you are posting a Sleepyhead Daily Detail graph on the forum, it should be minimized. To minimize the monthly calendar, just click on the triangle to the left of the current date. This is described in SleepyHead Chart Organization
If you click on a date in the calendar, the daily data for that date loads into the daily data window. It's also important to understand that the data for June 20, 2014 is the data for the NIGHT that started on June 20, 2014 and ended on the morning of June 21, 2014. And that's true regardless of whether you get to bed before midnight.
Now look at the little arrows in the calendar. The two arrows in green circles on the bar with the month's name allow you to navigate around the calendar without changing the data in the graphs. This makes it faster to get to a certain day you know you want to look at when it's not in the current "month". The two arrows that surround the bubble with the highlighted date for the daily data move one day backward or forward in data. The third outside arrow on the far right will immediately jump to the last date with data.
Pressing the downward triangle between the month and the year allows you to quickly change to a different month. Clicking the year allows you to quickly change to a different year. That helps if you need to jump to a date that is fairly far from the one you are currently looking at.
Pressing the upward facing arrow in the bubble with the the date in it will hide the calendar and change that triangle to a downward facing triangle. Clicking the downward facing triangle will unhide the calendar. Hiding the calendar is useful if you want more room for the Left Sidebar data.
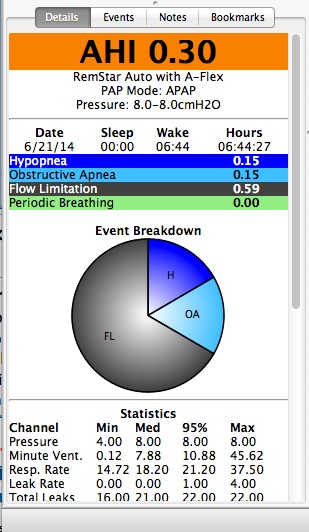
The Left Sidebar
The Left Sidebar has both summary data and statistical data for the given date. Typically you need to scroll down to see all the data.
Here's a picture showing the top part of the Left Sidebar Please read SleepyHead Chart Organization for tips on organizing the Left Sidebar without the pie chart or calendar for posting on the forum:
And here's a picture showing the bottom part of the Left Sidebar:
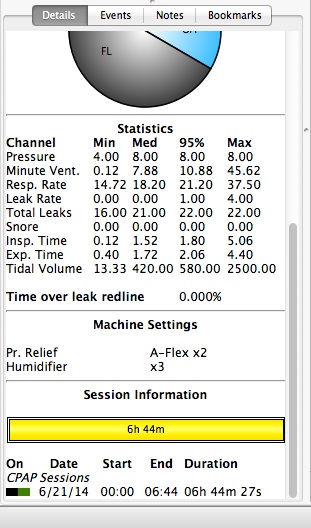
Tips on how to interpret all this data can be found in 4. Basic data interpretation: Daily Detailed Data. The organization of the Left Sidebar is what we're interested in here.
The top of the Left Sidebar is the summary efficacy data for the night. Below that is a pie chart that give the relative sizes of each of the major types of events scored by the machine. The pie chart can be turned off if preferred.
Below the pie chart is the statistical data for pressure, leaks, and respiratory data that may not be of much interest, particularly if you are just starting out.
Below the statistical data is some summary data about the machine's settings for the night and the session data. This data is from someone who typically turns the machine on, goes to sleep, and doesn't wake up until morning. For those with insomnia, session data is much more interesting.
The daily detailed graphs
The Daily data window. These are the graphs that the experienced forum members keep referring to when they ask for more specific information about what your graphs look like.
Here's a close up of the top of the graphical data:
The top chart is the Events chart. The Events chart gives a snapshot of just how good or bad the night was. (This patient had a really good night on this night). In SleepyHead 0.9.5 and 0.9.6, this chart is pinned to the top of the detailed data graphs and it will NOT scroll out of view when you scroll down to look at more graphs. It's best to leave the Events chart pinned since it serves as a navigation guide: The Events chart does not zoom in with the rest of the graphs.
The Flow Rate graph is often called the wave flow data. When you zoom in on this graph you can see a trace of every breath you took all night long.
The labels on the rest of the graphs are self-explanatory once you know the jargon. This is discussed later in this article.
Scrolling down reveals additional daily data graphs:
The particular graphs that you will see in SleepyHead depends on the machine you are using and whether you have turned any of the available graphs "off". This is discussed later in this article as well.
That gives a pretty complete picture of the overall organization of the data in SleepyHead. So you should now be able to find things pretty quickly. Understanding that data will be discussed later in this article.
Basic data interpretation: Daily Detailed Data
The amount of data available in SleepyHead can be overwhelming to new CPAP users, particularly those who only want some reassurance that "things are working." While many newbies tend to focus on the data in the Statistics tab and the Overview tab, the data in the Daily tab is usually more useful when you are trying to analyze what's going well and what's not going so well during the CPAP adjustment period. Moreover, the Daily Detailed Data is currently more robust and less buggy than the data presented in the Statistics tab. So I would encourage new SleepyHead users to first concentrate on getting comfortable with their detailed Daily data. Even so, you want to look at the detailed Daily data in context: One bad night does not mean things are suddenly not working; a month of bad nights does indicate something is wrong.
Most of the focus in this article is on how the daily data looks for ResMed and Philips Respironics machines. But most of it still applies to the data SleepyHead shows for any of the machines that it supports.
This article is primarily restricted to the most basic, important data for a newbie to concern themselves with. The focus is mainly upon the graphical data in the Daily Data window.
Left Side Bar data---AHI and event data table
- The left side-bar consists of
- The current date
- AHI Summary
- Settings Summary
- Session Starting, ending and total times
- Event rates per hour
- Statistics for pressure, leaks, snores and respiration
- Machine Settings Details
- Session Information
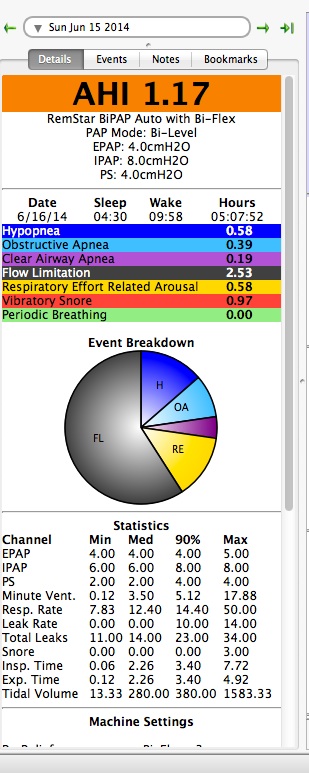
The Left Side Bar of the Daily data looks like this:
The most important piece of numerical data is the AHI data, however everything in the left side bar can provide clues on the effectiveness of your therapy. The goal of CPAP therapy is to improve the continuity and quality of your sleep by keeping the AHI down below 5 night after night.
If your AHI looks good and your leak data is acceptable, then the CPAP machine is doing its job. Whether that's enough to make you feel great is another issue, but the machine is doing its job.
Under the AHI banner we see the indices for all the various types of "events" that might be recorded during the night. In other words, the line that says
- Obstructive Apnea 0.39
means that the patient's OAI = 0.39 on this night. In other words
OAI = (number of OAs scored)/(run time) = 0.39
on this night.
If a particular type of event is not present in this table either your machine doesn't record them OR you didn't have any of those events on that night.
If your AHI is still too high and you ask folks on the forum about it, people will ask you about the distribution of events. They want to know what the OAI, the HI, and the CAI are. Note that
AHI = OAI + HI + CAI
In general the advice people will offer you about what to do about an AHI that is too high will depend on what the OAI and CAI look like.
Large Leak Summary Data
If you have any Large Leaks, SleepyHead will report the percentage of time spent in Large Leak territory with the other summary event data. This should make it easier for users to figure out whether their leaks are are significant enough to adversely affect therapy. Leaks are a problem when they are large enough to prevent effective pressure from being delivered, reduce feedback to the machine's sensors, or are disruptive to sleep.
The pie chart at the end of the index data gives a quick visual impression of what kind of events were most common. On this night the patient had far more FLs than any other kind of scorable event. The information on the Pie Chart is the same as the information on the Event Bar Charts. We suggest turning off the pie chart because it uses a lot of vertical space that could be used for other statistical information (see SleepyHead Chart Organization.
Note: ResMed machines record the snore data and flow limitation data as a continuous graph, so there will be NO snore data or flow limitation data on this table. RERAs are currently scored by Philips Respironics Dreamstaton CPAP and BiPAP machines, and Resmed Airsense 10 Elite or Autosets.
===IMPORTANT NOTES about Philips Respironics System One machines:===
1) The Philips Respironics System One machines record two kinds of Snore Data. In SleepyHead they are referred to as VS1 and VS2 data.
- In current versions of SleepyHead, The Vibratory Snore index shown in the Left Sidebar data is the average number of VS2 per hour. In other words:
- Vibratory Snore (index) = (number of VS2 scored)/(run time)
- In SleepyHead 0.9.3, The Vibratory Snore index shown in the Left Sidebar data is the average number of VS1 per hour. In other words:
Vibratory Snore (index) = (number of VS1 scored)/(run time) The thing is: VS1 snores are scored on a Philips Respironics machine only if the machine is running in Auto mode. If you are using a Philips Respironics machine in fixed pressure mode, the SleepyHead 0.9.3 Vibratory Snore index will always be 0.0; but that does NOT imply that you are not snoring.
2) The Flow Limitation data is recorded on a Philips Respironics machine only if the machine is running in Auto mode. If you are using a Philips Respironics machine in fixed pressure mode, the Flow Limitation index will be 0.0; but you can't assume that means you are not having any flow limitations.
Left Sidebar Data---Statistical Data chart
This is located directly below the Pie Chart. Let's look at it more closely:
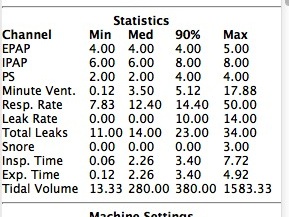
Med (Median) and 90% (or 95%) are statistical terms. The median value for a given set of data is the halfway point: Half the data is AT or BELOW the median value; half the data is AT or ABOVE the median value. The 90% value is the data value for which 90% of the data is AT or BELOW the value and 10% of the data is AT or ABOVE the value. Both Median and 90% are explained very carefully in a blog post Average, Median, 95% numbers: A guide to those who don't remember their introductory stats
Of all the numbers in this table, the most important ones are the Pressure numbers and the Leak and Total Leak numbers. All the other numbers in this table can safely be ignored.
The example patient uses a BiPAP and that's why there is both an IPAP and and EPAP line. The patient also uses a Philips Respironics machine, so that's why there is both Leak and Total Leak data. Users of a S9 Elite or AutoSet will see both lines for both pressure and EPAP, where the EPAP data equals Pressure - EPR. ResMed users will NOT have a line for Total Leak data since the S9 records only the unintentional leak data.
The EPAP line of the table looks like:
EPAP 4.00 4.00 4.00 5.00
This means that the patient's minimum EPAP =4, their median EPAP = 4, their 90% EPAP = 4, and their max EPAP = 5. What this tells us is that their EPAP stayed at 4cm for at least 90% of the night. But the EPAP did get as high as 5cm at some point during the night.
The IPAP line of the table
IPAP 6.00 6.00 8.00 8.00
means that the patient's minimum IPAP = 6, their median IPAP = 6, their 90% EPAP = 8, and their max IPAP = 8. That means that their IPAP stayed at 6cm for at least 50% of the night and the IPAP was LESS THAN or EQUAL to 8 cm for 90% of the night. From this data, we can't tell if the IPAP = 8 for almost 50% of the night or if the IPAP = 8 for only about 10-15% of the night.
Statistical Leak Data
The most important data in statistical data is the Leak data. Because the patient uses a Philips Respironics System One, there are two lines of leak data and they look like this:
Leak Rate 0.00 0.00 10.00 14.00 Total Leaks 11.00 14.00 23.00 34.00
The Leak Rate numbers are SleepyHead's statistical "guess" about what the patient's unintentional leak rate is. This number is NOT an official Encore number and it does not come directly from the data on the SD card; it is calculated from the Total Leak rate data that is recorded on the SD card.
The Total Leaks line is the statistical summary of the (raw) leak data. In some sense this may be more trustworthy for people using machines that record total leaks.
And the meaning of the numbers? The patient's median (unintentional) leak rate is 0.0 L/min, their 90% (unintentional) leak rate is 10.00 L/min, and their maximum (unintentional) leak rate is 14.00 L/min. This means:
- For at least 50% of the night, the unintentional leak rate was 0.0 L/min; in other words for at least 50% of the night, the patient had no detectable unintentional leaks
- For 90% of the night the leak rate was at or BELOW 10.00 L/min and for at most 10% of the night the patient's leak rate was ABOVE 10.00 L/min
- Since the maximum leak rate was 14 L/min, we know that for at most 10% of the night the patient's leaks were between 10 L/min and 14 L/min.
These Leak numbers are pretty good numbers for a Philips Respironics System One user.
The Total Leak numbers confirm that the patient's leaks are pretty well under control: The minimum total leak rate was 11.00 L/min; the median total leak rate was 14.00 L/min; the 90% total leak was 23.00 L/min; and the maximum total leak rate was 34.00 L/min. At the pressures used by the patient, the expected leak rate for their mask is about 20-29 L/min. So these numbers look very good: For 90% of the night the patient's total leak rate was AT or BELOW 23 L/min, which is right around the expected leak rate for their mask.
Time over leak redline
For ResMed users, SleepyHead will report the percentage of time when the Leaks are over the ResMed RedLine at 24 L/min at the end of the Statistical data under the Pie Chart. This should make it easier for ResMed S9 users to figure out whether their leaks are are significant enough to adversely affect therapy. Users of other CPAP machines will not have this line in their Daily Data report.
Part I: Are my leaks bad enough to worry about? Interpreting the statistical leak data
If you use a Philips Respironics or ResMed, SleepyHead will show you the percentage of time your leaks were in Large Leak territory for your machine. This will help you evaluate whether or not your excess leaks are both large enough and long enough to adversely affect your therapy. A small amount of time in Large Leak territory can be ignored if your leaks are under control for most of the night; a large amount of time in Large Leak territory cannot be ignored.
The question is: How much time in Large Leak territory is too much? ResMed provides a guideline for its users: Mr. Red Frowny face shows up on the Sleep Quality Report if your leaks are above the Redline for at least 30% of the night. When the Large Leaks last that long, ResMed's engineers believe both efficacy of the CPAP therapy and the accuracy of the recorded data can be adversely affected. We will assume that 30% of the night in Large Leak territory is clearly bad news for users of any CPAP machine. But many people may find that their therapy begins to be compromised by the time Large Leaks make up 20% of the night. For a lot more information on leaks, see 8. Leaks.
If you are using a DeVilbiss IntelliPAP or an Fisher & Paykel Icon, then you will need to use the median and 90% (or 95%) Leak/Total Leak data to evaluate your leaks.
In order to make sense of the statistical numbers shown on the Leak Rate and Total Leaks lines, you need to know how the manufacturer of your machine defines Large Leak. Information about how ResMed, Fisher & Paykel, DeVilbiss define Large Leak can be found in 8. Leaks. Philips Respironics does not have a published "line" for defining Large Leak on the System One machines, but there are patterns that have been noticed in the Philips Respironics data. That information is also talked about 8. Leaks.
In general: If your maximum Leak or Total Leak data is well under the official Large Leak definition for your machine, then you know you do NOT have any leaks that are large enough to clearly affect the efficacy of your therapy or the accuracy of your data.
If your 90% (or 95%) Leak or Total Leak data is well under the official Large Leak definition for your machine, but the maximum Leak or Total Leak data is over the Large Leak line for your machine, then you have a few, probably short lived Large Leaks. At most your leak was in Large Leak territory for no more than 10% (or 5%) of the total night. Unless all the time in Large Leak territory is in one prolonged Large Leak, chances are your Large Leaks are NOT long enough to have an adverse affect on your therapy.
If your median Leak or Total Leak data is well under the official Large Leak definition for your machine, but the 90% (95%) Leak or Total Leak data is near or over the Large Leak line for your machine, then you may have a leak problem that is both large enough and long enough to adversely affect your therapy. On the one hand, we know that your leak was NOT in Large Leak territory for at least 50% of the total night. But the numbers alone don't tell us if you were in (or close to) Large Leak territory for only 10-15% of the night or if you were in (or close to) Large Leak territory for 45% of the night. You really need to examine the leak graph to figure out what's going on. More on that later.
If your median Leak or Total Leak data is close to or above the official Large Leak definition for your machine, then you definitely have a problem with Large Leaks. You are leaking at a very high and significant rate for at least 50% of the night, and that definitely means that the leaks are both long enough and large enough to adversely affect your therapy and the accuracy of your data.
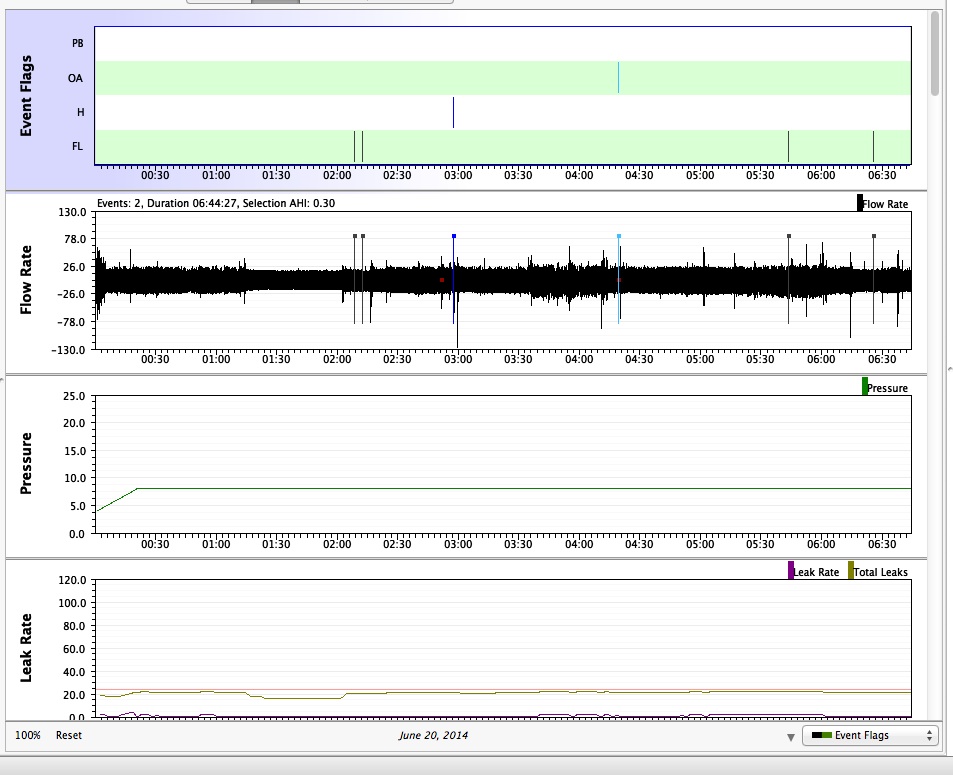
Important Daily Detailed Graphs
The machine you are using will determine exactly which graphs will show up in your Daily Data. But the most important graphs will be present in every machine's data.
In SleepyHead you can temporarily hide unneeded graphs so that they're not in your way; resize graphs so that more of them fit on your screen; and rearrange the graphs so that you can group the graphs you want to look at together. You can also pin selected graphs to the top of the Daily graphs section so they do not scroll out of view. You can also zoom in on particular parts of the data where there is a lot of activity so that you can get a better idea of what might be going on at night. Instructions on how to do all these things can be found in 13. Manipulating Daily and Overview Graphs.
This article concentrates on which graphs are important, what information they convey, and how they are related to each other.
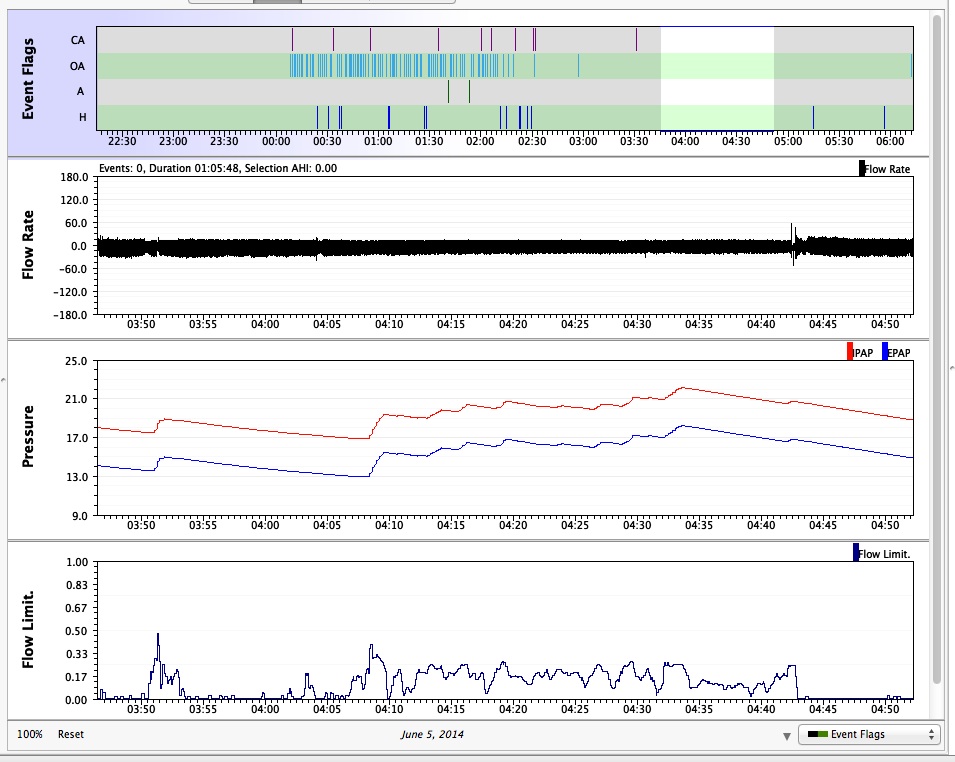
First a screen shot of the preferred set up of the daily graphs:
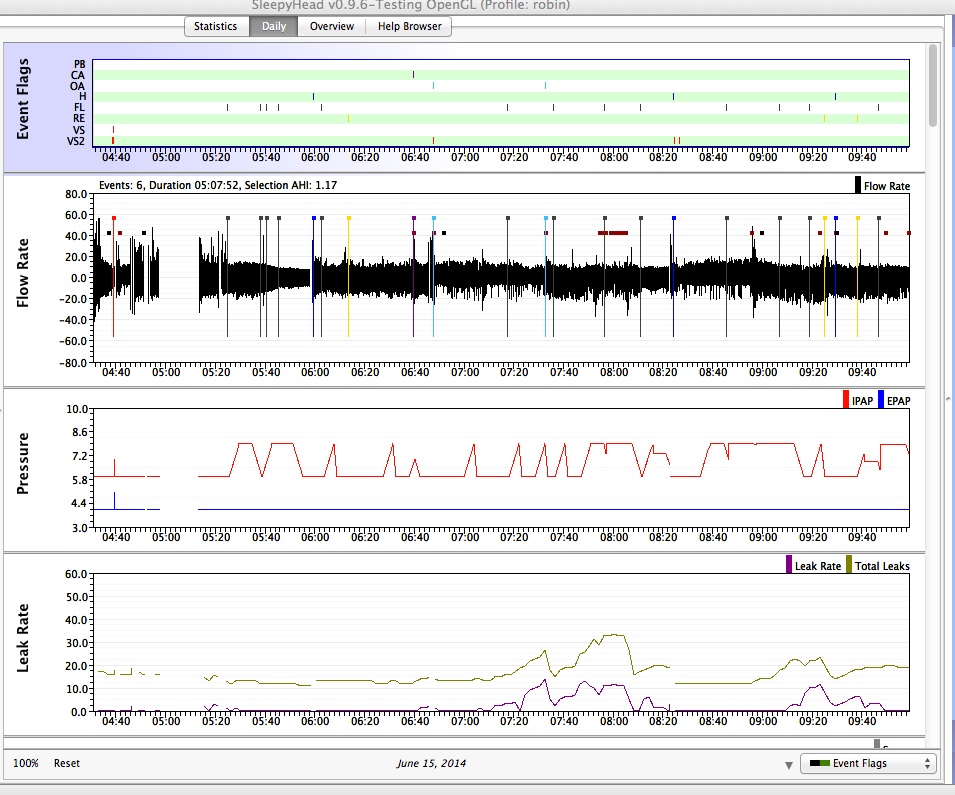
This screen shot shows the four most important Daily Detailed graphs that are needed to have a clear understanding of your data and what's going on each night.
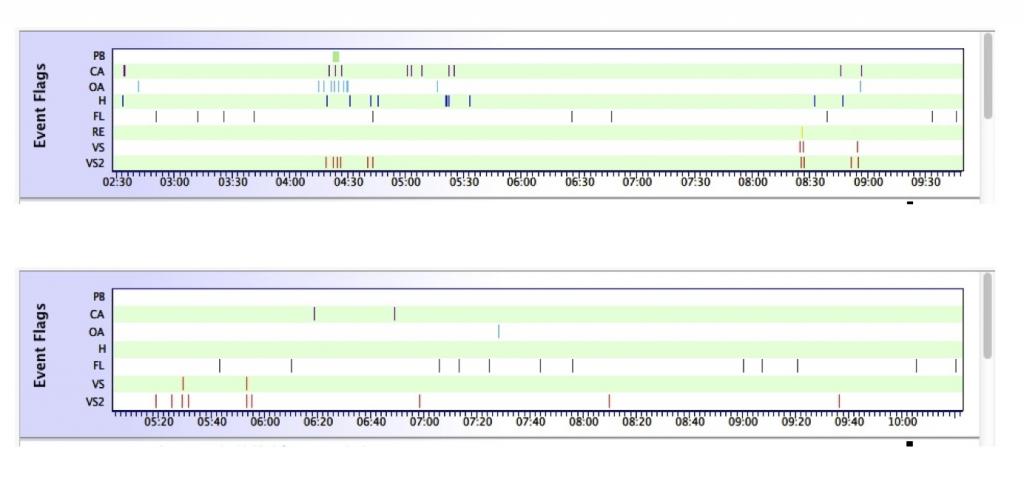
The Events Table
The Events Table is a snap shot that lets you see when all the events occurred and what kind of events they were. By default, the Events table is pinned to the top of the Daily Detailed Data graphs and will not scroll out of site. When zooming in on the other graphs, the Events Table will remain as is, with the zoomed in part of the night highlighted on the events table. So it also provides a useful reference tool for being able to quickly put the zoomed in graphs into the context of the whole night.
The Flow Rate graph
NOTE: ResMed S9, Philips Respironics System One, and Fisher & Paykel Icon machines record Flow Rate data if the card is in the CPAP machine during the night; the DeVilbiss IntelliPAP does NOT record Flow Rate data.
The Flow Rate graph is also referred to as the "wave flow" graph. It provides a record of each and every breath you took all night long. At this scale, everything is all run together; the real power in the Flow Rate graph is when you zoom in sufficiently close to start seeing individual breaths and events. Note that each of the events in the event table shows up as a tick mark on the Flow Rate graph (with the exception of the Philips Respironics System One VS2 tick marks.) The little boxes appearing on the sample patient's Flow Rate graph are mostly Pressure Pulses that the Philips Respironics central detection algorithm uses for testing the patency of the airway.
The Pressure graph
The Pressure graph shows the therapeutic pressure level throughout the night. Because this particular patient uses a Philips Respironics BiPAP, the IPAP and EPAP graphs vary independently of each other. The IPAP is the top graph; the EPAP is the lower graph. ResMed Elite and AutoSet users will have two pressure graphs if they have EPR turned on. The top graph is the Pressure setting; the bottom graph, which is label EPAP, shows what EPAP = Pressure - EPR looks like.
If you are using your CPAP in fixed pressure mode, the pressure graph is not of much use---unless you are spending a lot of time hitting the ramp button. But if you are using your CPAP in Auto mode, the pressure curve tells you when the machine raised the pressure and how much it raised the pressure. Comparing the pressure increases with the events flagged in the Flow Rate curve or the Events Table can give you some very good ideas about why the machine decided to increase the pressure and also give you a sense of whether the disordered breathing got better or worse with the pressure increase.
The Leak Rate graph
This graph shows both the Total Leaks (light gold color on top) and the SleepyHead calculated (unintentional) Leaks (purple on bottom) because I'm using a Philips Respironics System One. A ResMed user is only going to see the purple Leaks graph.
In this example, the Redline option turned OFF because the patient knows her leaks well enough to know that an official Encore LL is going to be scored only if the Total Leak Rate is up near 60 L/min.
This is not the patient's best leak line, but it is a perfectly acceptable leak line for a Philips Respironics System One BiPAP with IPAP = 8 and EPAP = 4 or 5.
Looking at the Leak graph will allow you to see just how long your worst leaks lasted and just how big they were. When the leak graph looked at along with with the statistical leak data in the Left Sidebar, you can get a very good idea of whether leaks may be adversely affecting your therapy. If you have a wide Auto range, you can track whether increases in pressure are leading to increased unintentional leaking. And when the leak rate is in Large Leak territory, you can often see how the Large Leak affects the ability of the machine to track the breathing, and how that affects the accuracy of the AHI data.
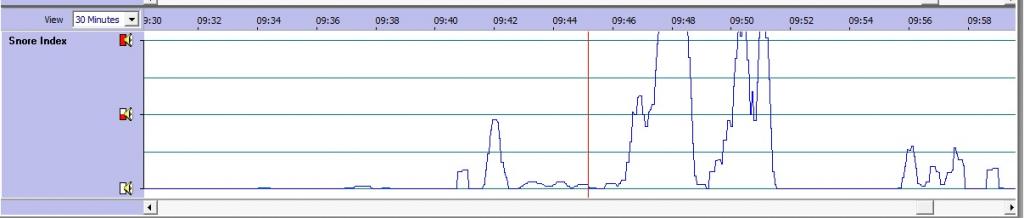
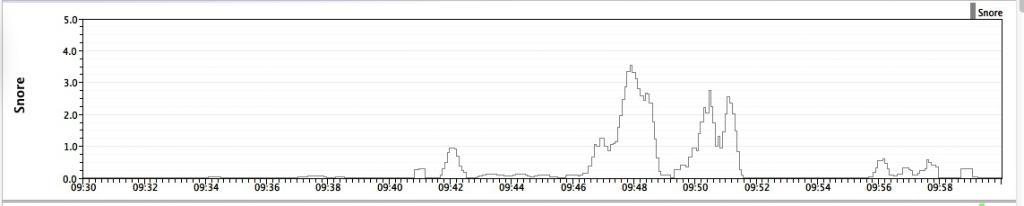
The Snore graph
The snore graph is sometimes useful to look at, even though no-one knows just what the y-axis numbers actually mean. The reason its useful is that snore graph can sometimes explain a pressure increase when there seems to be nothing unusual going on in the Flow Rate graph. The presence of snores can be a predictor of obstruction and cause auto CPAP and BiPAP machines to increase pressure.
The Flow Limitation Graph
For ResMed, the Flow limitation graph is sometimes useful to look at because it can explain a pressure increase in the absence of both snoring and events. High spots on the Flow limitation graph typically correspond to some pretty distorted looking inhalations in the Flow Rate graph. Flow limitation is an important component of pressure increases in auto CPAP and BiPAP machines.
NOTE about Flow Limitation data: The Philips Respironics machines score FL in a very different way than the ResMeds do, and this means there is no FL graph for a Philips Respironics machine.
ALL OTHER GRAPHS
All the other graphs (the Respiratory Rate, the Tidal Volume, the Minute Ventilation, and so on and so forth) can be ignored by newbies. If there's something really odd in your Flow Rate data, a more experiences forum member may ask you for one of these graphs on occasion. If you're a real data junkie, you may find these graphs interesting, but they usually do not provide much help in figuring out what might be wrong when a newbie is in trouble. These graphs will be discussed later.
The Event Table---a detailed look
The Event table gives a snapshot of how good or bad the whole night was, and whether certain parts of the night were much uglier than the overall AHI might indicate. Compare these two event charts:
You don't need the actual AHI numbers to see that the first night was a lot worse than the second. On the second night, there are only three "events" scored all night: Two CAs and one H. There are a few Flow Limitations, which are common in this patient's data), but even the FL are well spaced. And the bit of snoring at the beginning of the night is not a real issue. Overall, this night's efficacy data is really quite good.
But on the first night, there are a lot more tick marks over all AND between 4:15 and 5:30 there are a lot of OAs, Hs, and CAs scored. There's a second smaller cluster of events around 8:30 as well. The other thing we can immediately see about the first night is that outside of the 4:15-5:30 and 8:30-9:00 time frames, the rest of the night was pretty good.
The Event table tells us where to look if we want (a lot) more information about periods with "bad night-time breathing." On the top night's data, it's worth zooming in on the 4:15-5:30 to see just how ugly things are. When we zoom in on the daily graphs, the Event table remains fixed, but the zoomed in time frame is highlighted as shown:
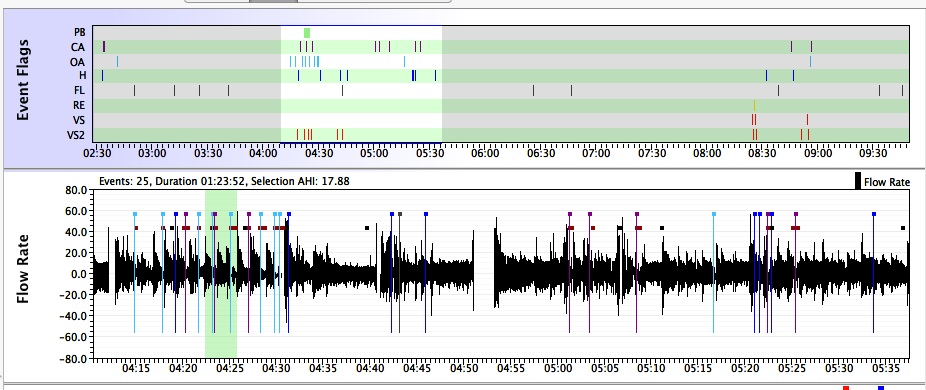
The highlighting on the Event table gives a quick visual reference of where the zoomed in data comes from. That's useful if you start scrolling through zoomed in Flow Rate data for a whole night and notice something of interest. In other words, the Event Table serves as a "navigation" tool when you are looking at zoomed in detailed data.
Because the Event Table provides both an overall snapshot of the whole night AND serves as a navigation tool, in SleepyHead 0.9.6, the Event Table's positions is pinned at the top of the Daily Data graphs.
When posting screen shots of zoomed in Daily Data, it is useful to include the Events Table in the screen shot so the others can get a sense of how the selected Detailed Data fits into the night as a whole.
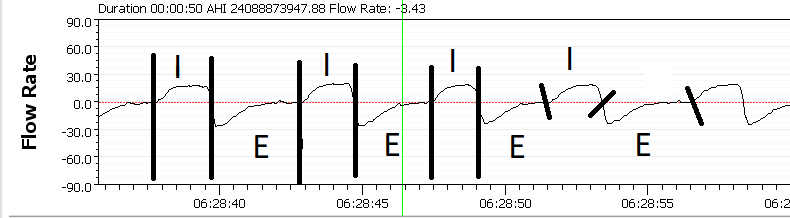
The Flow Rate graph---a detailed look
NOTE: Not all machines produce detailed flow rate graphs.
The Flow Rate graph is a visual record of each and every breath you took while using the machine. You are inhaling when the Flow Rate is positive and you are exhaling when the Flow Rate is negative. Stronger inhalations result in higher (positive) peaks and stronger exhalations result in lower (more negative) valleys in the Flow Rate graph. The events from the Event Table are superimposed on the Flow Rate graph with vertical lines of different colors.
The Flow rate graph can be enhanced by showing a dotted line at zero flow by right-clicking on the left margin of the Flow Rate Graph and using the context menu to set a Dotted Line at Zero. Everything above that line is inspiration (I) and everything below is expiration (E). This is a good example of normal I:E where in inspiration time is shorter than expiration. Normal breathing in this case, the inspiration quickly gains in flow rate (volume in mL/sec) and reaches a peak at which time the flow rapidly slows to zero, then expiration seamlessly beings. The expiration cycle is passive, meaning your chest simply relaxes and gravity does most of the work of collapsing the chest and causing air in the lungs to flow out. Expiration results in a fast flow rate at first which gradually slows to near zero resulting in the flattened line near zero flow. This is not holding your breath, but is the result of a relaxed normal exhale, as compared to a forced exhale. Take a look at your figure with the transitions from I to E marked. We can look at the transitions in the time scale (x-axis) and see that inspiration is approximately one breath every 5-seconds (12 BPM) with inspiration being about 2.2 seconds and expiration being 2.8 seconds. Notie the green line bisecting the graph during expiration below and showing -3.43 mL/sec flow. This shows the exact place where your cursor was located is indeed in expiration and there is expiratory flow. This would be textbook normal.
Inspiration Expiration Ratio (I:E Ratio)
The usual way of expressing the I:E ratio is to compare inspiration time to expiration time. The best statistic to use for calculating the I:E Ratio is the median inspiration and expiration times. For example median values from your data, assume your inspiratory time is 1.54 and expiratory time is 2.88. 2.88/1.54=1.87, or a ratio of 1 to 1.87 (Also expressed as 1:1.87). In this case, the expiration is nearly twice as long as inspiration which is normal. In general, the I:E ratio will range from 1:1 to 1:3, meaning normal exhale can be in a range of equal to 3 times the time of inhale.
We often see an I:E ratio of less than 1 suggesting a longer inspiration time than expiration. This inverse I:E ratio can occur, but most of the time it is an error in the respiration timing by the CPAP machine. In most cases, the machine will count part of expiration as inhale, resulting in an incorrect I:E time or ratio. An I:E ratio must be greater than zero and generally greater than 1:0.5 (one to one-half seconds), and will usually be less than 1:3 (one to three-seconds). Please note that Sleepyhead and OSCAR currently show incorrect I:E times on all Philips CPAP and BiPAP machines because inspiration starts when flow returns to zero from expiration. Work is in progress to correct this error by changing the inspiration signal to a positive flow rate. Resmed machines generate the I:E data and it can be considered reliable.
Robysue's Flow Rate Interpretation from Forum Posts
The Flow Rate graph looks quite different depending on how far you have zoomed in on the data. All of the following Flow Rate graphs are from the same night's data:
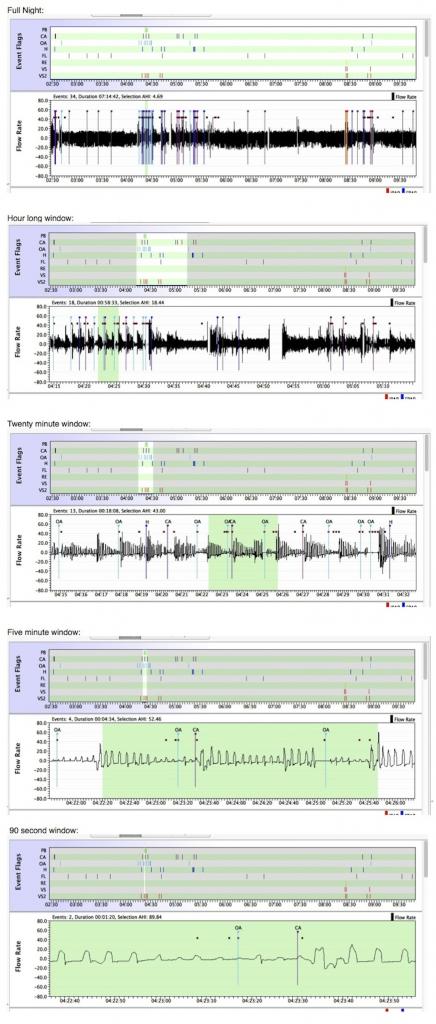
Different information is conveyed by different levels of "zoom" in the Flow Rate graph. More information on the Flow Rate graph can be found in 9. Beyond AHI: Getting specific information about events.
For now we will give the following broad guidelines about looking at the Flow Rate graph at differing zoom levels:
- Full night. This usually doesn't give much more information than just the events table. But sometimes you can get a sense of when you were particularly restless because normal sleep breathing is usually much more shallow than normal wake breathing. If there are a lot of places with really big values for the wave flow, those may indicate restless periods during the night.
- 60-90 minute windows. These usually let you see what's going on during a full cluster of events, but they usually don't let you see what's going on at the individual breath level. Sometimes you can spot funky breathing patterns that might be indicative of unstable respiration patterns that are common in periodic breathing or potential CO2 undershoot/overshoot cycles; sometimes you can't.
- 5-20 minute windows. You can see the individual breaths, and for many clusters, a 20 minute window will show you the whole cluster.
- 30-60 second windows. You can see an individual event, but not much else. Unless you have a question about a specific individual event, zooming in this far usually results in not giving enough context to others to evaluate the data and provide intelligent feedback.
Additional notes about navigating inside the Flow Rate graph
These comments apply to ALL the Detailed Daily Data graphs except for the Event Table, but for the most part, you need these tips when you're examining the Flow Rate graph.
1) Zooming and unzooming: You can zoom in on the center of the Flow Rate graph by LEFT clicking when the mouse is over the Flow Rate graph. You can zoom back out by RIGHT clicking when the mouse is over the Flow Rate graph.
2) Scrolling through a Flow Rate graph: Regardless of how far you have zoomed in on the Flow Rate data, you can scroll through the Flow rate graph by holding the RIGHT mouse button down while moving the mouse in a horizontal direction.
3) Glitches: Sometimes you run into a SleepyHead glitch and the y-axis for the Flow Rate graph is off: The middle part of the breathing cycle is not graphed at 0 L/min. It's a known problem. If this happens to you, the easiest thing to do is just to mentally draw the 0.0 L/min line half way between the peaks and valleys in the Flow Rate graph and use that to measure when you are inhaling and exhaling.
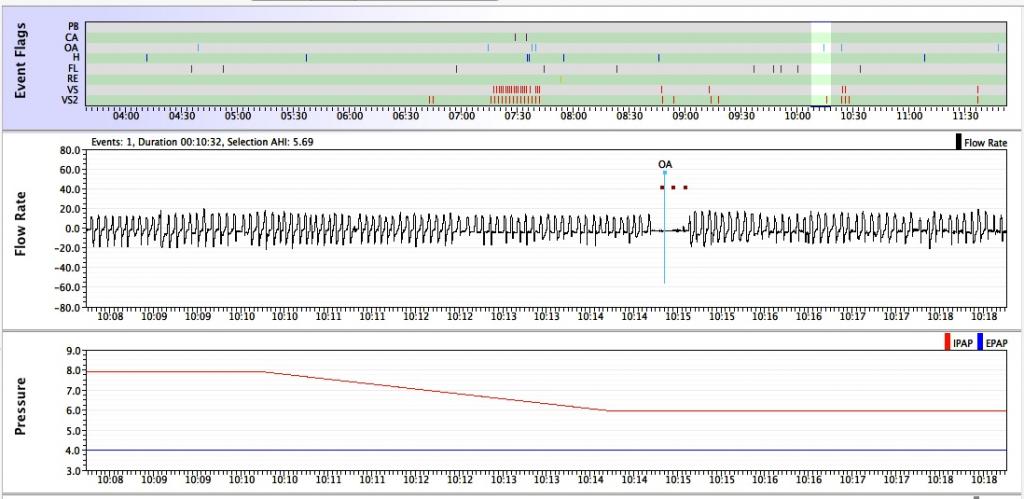
The Pressure graph---a detailed look
If you use a CPAP or APAP that is NOT a ResMed S9 Elite or S9 AutoSet, you will only see one pressure curve. If you use a bi-level device OR a ResMed S9 Elite or S9 AutoSet, you will see two curves. The top curve is the IPAP---the pressure setting for inhalations; the bottom curve is the EPAP---the pressure setting for exhalations. (The reason the S9 Elite and AutoSet have two pressure curves is that when EPR is on, the machine acts very much like a bi-level.)
If you are using your CPAP in fixed pressure mode, the Pressure graph will be a flat line after the ramp period is over. Hence the Pressure graph provides no useful data and can be ignored. So for this section, we will presume that you are using an auto adjusting machine and that it set to Auto mode.
The primary data you can get off the pressure curve is information about what the machine thinks your pressure needs seem to be for the night. Looking at the Pressure graph and the Flow Graph together allows you to see just how the machine responds to your sleep apnea each and every night. (On a ResMed S9 AutoSet, you might also need to look at the Snore graph and the Flow limitation graph as well.)
Common concerns that people have about their Pressure graph
Most concerns and questions people tend to ask about the Pressure graph are really about the Pressure graph relates to other parts of the data. Here are some common things people ask concerning the Pressure graph.
Question: I had an OA and the machine didn't increase the pressure. Why didn't it increase the pressure to blow through the event and open my airway and end the apnea?
Answer: While APAPs and Auto bi-levels are designed to respond to OAs with pressure increases, they are NOT non-invasive ventilators and they CANNOT trigger inhalations. (The fancier ASV machines ARE non-invasive ventilators and can trigger inhalations). If the machine is going to increase the pressure in response to an OA, it will wait until the OA is over and you are breathing again before it increases the pressure.
Moreover, the auto-algorithms are designed to NOT respond to isolated OAs and Hs: Unless two or more events happen relatively close to each other (as in within about 2 minutes of each other), an APAP or Auto bi-level machine is programmed to NOT increase the pressure. Here's an example of a 20-second OA that a patient's BiPAP Auto ignored:
You'll note that the machine had been decreasing the IPAP pressure (since the breathing was stable) for several minutes before the OA occurred. Neither the patient's EPAP (which is at its minimum value) nor their IPAP is increased for this particular OA because it's isolated. There's not another OA or H within 2 minutes of this particular OA.
The fact that APAPs and auto bi-levels do not respond to isolated OAs and Hs seems counter-intuitive to many new CPAP users. But this lack of response is intentional and it mimics the AASM Clinical Guidelines for Manual Titration Sleep Studies. The idea is not to jack up the pressure every time any event happens: That can lead to more unstable breathing, discomfort, and more pressure than is needed to keep the airway open most of the time.
Question: Why is my pressure increasing when there don't seem to be any events?
Answer: APAPs (and Auto bi-levels) increase pressure in response to OAs, Hs, snoring, and flow limitations. The Philips Respironics System One APAP and BiPAP Auto also increase pressure in response to RERAs. The Philips Respironics System One also has a "search" routine built into its Auto algorithm, and it will periodically increase the pressure as a "test" to see if the shape of the wave flow improves, even if nothing is being scored. Those test increases show up as saw-teeth on the pressure curve. On ResMed machines, the most likely cause for a pressure increase without any events is probably snoring or flow limitations. Here's a picture of a increase in pressure on a ResMed VPAP in response to nothing but flow limitations:
While this person had a ton of OAs scored early in the night (along with some dramatic pressure increases), the snippet we're looking at here shows two pressure increases in response to activity on the Flow Limitation graph. The second pressure increase starts a bit before 4:10 and doesn't end until a bit before 4:35. In those 25 minutes, the S9 increases the pressure by a full 5 cm without an OA or H in site.
Question: If I'm having a lot of events and my machine is running at or near its maximum pressure setting a lot of the time. Does that mean I need to increase the max pressure?
Answer: It depends.
Looking at the Pressure graph, along with the Flow Rate graph and type of events being scored all come into play in figuring out what might be the best course of action. Sometimes it's pretty easy to tell when a modest increase in either the min or max pressure setting is a reasonable thing to try. But sometimes things are not so simple.
On the one hand, the maximum pressure setting needs to be high enough to effectively prop the airway open during the times when the airway is most likely to collapse. If the maximum pressure is not high enough, the airway will continue to be prone to collapsing off and on throughout the night.
On the other hand, the minimum pressure needs to be high enough where the machine does not need to increase the pressure by a significant amount during the first cluster of events. Sharp rapid increases of 5-8 cm of pressure in 10 minutes might not allow the airway enough time to stabilize and settle down. And unstable breathing can cause further events, which leads to more pressure increases and more unstable breathing.
And then to muddy the waters even further: Approximately 10-15% of CPAP users may have a tendency to develop pressure-induced central apneas if the pressure setting is too high. And what "too high" is strongly depends on the individual. And while modern machines have algorithms to distinguish central apneas from obstructive ones, those algorithms are not perfect, and there is some evidence that the algorithms may be more likely to mis-score CAs as OAs when the CAs occur at relatively higher pressures.
So blindly increasing your pressure just because the machine is running at or near your maximum setting all night long is not a good idea. Before you decide to change your pressure settings, you really need to do some careful thinking about what you hope to accomplish by changing the pressure and have a plan on how to evaluate whether the change does what you intend it to do. And keep in mind that it really is a good idea to consult your sleep doctor about any changes to your therapeutic settings.
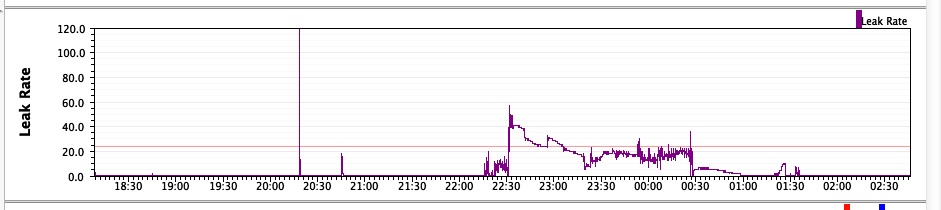
The Leak Rate graph---a detailed look
Depending on what machine you are using, the Leak Rate Graph will have either one or two graphs in it.
ResMed machines report only the excess leak rate, which is simply called Leak in the SleepyHead leak data. A ResMed user will see only one leak graph in the Leak Rate graph.
All other major brands of data-capable CPAPs report Total Leaks, which include both the intentional leak rate for your mask at your pressure AND the excess leaks. In other words:
Total Leak = Intentional Leak + Excess Leak
SleepyHead does a statistical analysis of the Total Leak data for non-ResMed machines to calculate an estimated excess leak rate and reports this estimated excess leak as Leak Rate. This means that users of NON-ResMed machines have two "leak" graphs in the Daily Detailed Data graphs: One for Total Leak (the raw data from the machine) and one for Leak (the SleepyHead estimated excess leak rate).
The top (gold) graph is the Total Leak Rate graph and the bottom (purple) graph is the Leak Rate graph, which shows the SleepyHead estimated excess leak rate.
Defining Large Leaks
Different manufacturers have different definitions of what Large Leak means for their machine. But for all brands of machines, the idea is that if your leaks are under the manufacturers Large Leak definition, the machine should be able to gracefully compensate for the leaks and deliver effective therapy and accurate data. Information about how ResMed, Philips Respironics, Fisher & Paykel and DeVilbiss each define Large Leak can be found in 8. Leaks.
Tools to help identify Large Leaks: Show Leak RedLine If the manufacturer of your machine has a published Large Leak definition, you can use the Show Leak Redline option to draw a Red Line on your Leak/Total Leak graph to make it easy to spot when the leaks are high enough to be considered Large Leaks. The Show Leak Redline option is talked about in 7. Important "preferences settings.
A typical SleepyHead 0.9.6 Leak graph from an S9 VPAP Auto that shows a night with one long leak that is in or near Large Leak territory is shown below. It's worth noting that the amount of time with the leak rate AT or ABOVE 24 L/min is only about 40 minutes and the total run time for the night was about 8.5 hours; hence Mr. Green Smiley Face showed up the next morning on the S9's LCD.
Tools to help identify Large Leaks: Large Leak shading for Philips Respironics System One machines
For users of Philips Respironics System One machines, SleepyHead 0.9.6 will use the Encore Large Leak data to identify parts of the Flow Rate curve that are earmarked as occurring during Large Leaks. The Large Leak will also show up on the LL line in the Events Table as a gray bar and it will show up on the Flow Rate graph as gray background shading. By looking at both the Flow Rate data and the Total Leak line, you can be begin to get a sense of where your Philips Respironics machine draws the Large Leak line for your mask and your pressures. An example of how SleepyHead 0.9.6 flags one patient's rare official Large Leaks is shown below. (This Large Leak has a number of really interesting characteristics, and you can read about it in the blog post, Anatomy of a Large Leak in Encore and SleepyHead, which analyzes exactly what's going on in this leak. )
Part II: Are my leaks bad enough to worry about?
Interpreting the graphical leak data
The Leak Rate graph is the most reliable way of answering the question: Are my leaks both large enough and LONG enough to adversely affect the quality of my therapy and the accuracy of my data?
Loosely, Leak and Total Leak lines can be described as "Great", "Good", "Decent Enough", "Problematic", "Bad", and "Horrible", all of which are based on the amount of time the leaks or total leaks are in Large Leak territory for your particular machine.
Great, Good, and Decent Enough Leak/Total Leak lines
In general, a Great Total Leak line will be flat or almost flat and hover somewhere around (or just below) the intentional leak rate for your mask at your pressure. A Good Total Leak line will be "fuzzy" flat, stay mostly around the intentional leak rate for your mask and pressure, but tends to have some visible periods of noticeably higher leaks, most of which stay well below the cut off for "Large Leaks" for the given machine. A Decent Enough Total Leak line has more obvious leaks than a "Good" one does, but line stays below the Large Leak line for at least 70-90% of the night. (There's some debate between CPAP users of just how long the Large Leaks need to last before they become problematic.)
For ResMed users or for folks who simply want to concentrate on the (excessive) Leak data, a Great Leak line will be flat or almost flat and hover somewhere around (or just below) 0.0 L/min. A Good Leak line will be "fuzzy" flat, stay mostly around 0.0 L/min, but tends to have some visible periods of noticeably higher leaks, most of which stay below 10-15 L/min. A Decent Enough Leak line has more obvious leaks than a "Good" one does, but the line stays below 25-30 L/min for at least 80-90% of the night. (There's some debate between CPAP users of just how long the Large Leaks need to last before they become problematic.)
If we look at the Statistical Leak data from the Left Side bar for Great Leak/Total Leak lines and Good Leak/Total Leak lines, the 90% (or 95%) Leak/Total numbers will be under the manufacturer's definition of "Large Leak". The maximum may or may not be under that line.
The Statistical Leak data for a Decent Enough Leak/Total Leak line will have a median Leak/Total Leak number well below the the manufacturer's definition of "Large Leak". The 90% (or 95%) leak numbers, however, may very well be larger than the official Large Leak definition.
Problematic Leak/Total Leak Lines
These are leak lines where it's clear that Large Leaks are present during a significant amount of the night, but it's not clear if the Large Leaks last long enough for the machine's manufacturer to say they are a problem.
The manufacturer with the clearest definition of when Large Leaks become long enough to adversely affect the quality of the CPAP therapy and the accuracy of the data is ResMed: ResMed's infamous Mr. Red Frowny Face shows up on the machine's Sleep Quality Report when the (excess) Leaks are AT or ABOVE 24 L/min for at least 30% of the night. So we'll assume that if the time in Large Leak is approaching 30% of the entire night, the Large Leaks are problematic.
So a good working notion for a Problematic Leak/Total Leak line would be the following:
A Problematic Total Leak line is one that is NEAR or IN the manufacturer's Large Leak Territory for somewhere between 20-35% of the night; A Problematic Leak line is one that is ABOVE 24 L/min for somewhere between 20-35% of the night. A Problematic Leak/Total Leak line indicates that the leaks may be both long enough and large enough to have an adverse affect on the quality of your therapy and the accuracy of the data.
The Statistical Leak data for a Problematic Leak/Total Leak line will typically have a median Leak/Total Leak number well below the the manufacturer's definition of "Large Leak", but the 90% (or 95%) leak numbers, will be larger than the official Large Leak definition.
If you see a Problematic Leak/Total Leak line every now and then, there's no point in worrying about it. If you see Problematic Leak/Total Leak lines a lot, however, you may want to consider taking measures to address the leak issues.
Bad and Horrible Leak/Total Leak Lines
These are leak lines where it's clear that that Large Leaks are present during substantial amount of the night, and it's clear the Large Leaks are both long enough and large enough to adversely affect your CPAP therapy.
A working definition of a Bad Leak/Total Leak line is that the leaks are bad enough to trigger a visit from Mr. Red Frowny Face if you were using a ResMed S9: If large leaks make up more than 30% of night, you've got a problem with leaks.
A Horrible Leak/Total Leak line is a leak line where the leaks are totally out of control: If over 50-60% of the night is in Large Leak territory, you've got a Horrible Leak/Total Leak line and a pretty significant problem with leaks.
The Statistical Leak data for a Bad Leak/Total Leak lines may have a median Leak/Total Leak number well below the the manufacturer's definition of "Large Leak", but the 90% (or 95%) leak numbers, will be larger than the official Large Leak definition. If the median Leak/Total Leak number is close to or above the the manufacturer's definition of "Large Leak", then you've got a Horrible Leak/Total Leak line.
Most people don't have random, rare Bad or Horrible Leak/Total Leak lines. Folks who have real leak problems tend to have Bad or Horrible Leak lines on a significant portion of the the nights they use the CPAP. If you are seeing multiple Bad or Horrible Leak/Total Leak lines each week, you know you need to do something about the leaks.
A final comment on the connection between the Statistical Leak data and the graphical leak data
It is important to note that Decent Enough, Problematic, and Bad Leak/Total Leak lines may all have the same characteristics in the statistical Leak data:
- The median Leak/Total Leak numbers will be well under the manufacturer's official definition of Large Leak
- The 90% or 95% Leak/Total Leak numbers will typically be above the manufacturer's official definition of Large Leak.
What separates Decent Enough leaks that you don't need to worry about from Bad leaks that must be fixed is the duration of the large leaks. And knowing the median and 90% leak/total leak rates is just not enough information to tell whether the large leaks lasted about 10-15% of the night (Decent Enough) or whether the large leaks lasted about 40-45% of the night (Bad or Horrible).
If the median Leak/Total Leak numbers look good and the 90% (95%) Leak/Total Leak numbers are in Large Leak territory, you must look at the Leak/Total Leak graphs in order to figure out whether the leaks were both long enough an large enough to adversely affect your therapy.
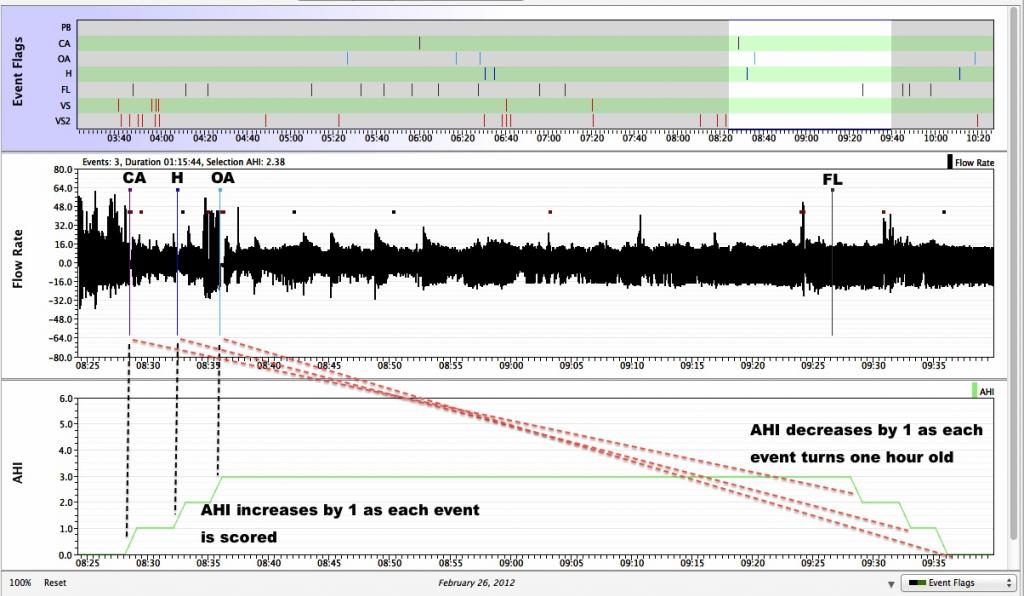
The AHI Graph
This graph is often misunderstood by many new CPAP users and because of that, we often recommend new SleepyHead users simply ignore this graph.
And yet, many newbies are very interested in this graph. So in the interest of trying to clear up misconceptions about this graph, it is included here.
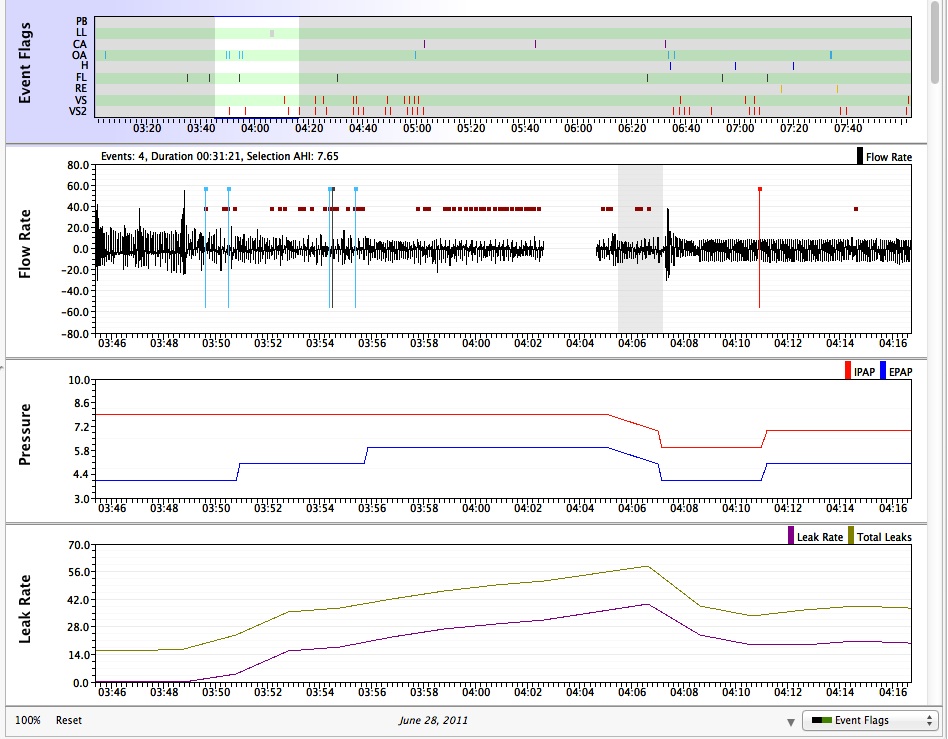
The y-value in the AHI graph gives running count of the number of apneas scored during the last 60 minutes of the current CPAP session. In other words, the y-value of the SleepyHead AHI graph at time t is the total number of events (OAs+CAs+Hs) recorded during the last hour of run time in the current session. When a particular event becomes one hour old, it is dropped from the running total. Because each event that is scored remains part of the AHI graph until it is an hour old, the AHI graph will remain above 0.0 for long periods of time when no events are being scored. The following image shows a series of 3 events scored within an 8-minute period, followed by over an hour of sleep with no additional OAs, Hs, or CAs scored. The AHI first increases to 3 and it stays at 3 until each of the three events "ages" out of the running total:
AHI Graph and its connection to the Flow Rate graph and the Events table:
A more complicated example.
When there is a lot of activity in flow rate data over a long period of time, what happens to the AHI graph may be more complicated. Here is a marked up copy of part of a patient's AHI graphs that show what can happen when multiple clusters of events occur within 90 minutes of each other:
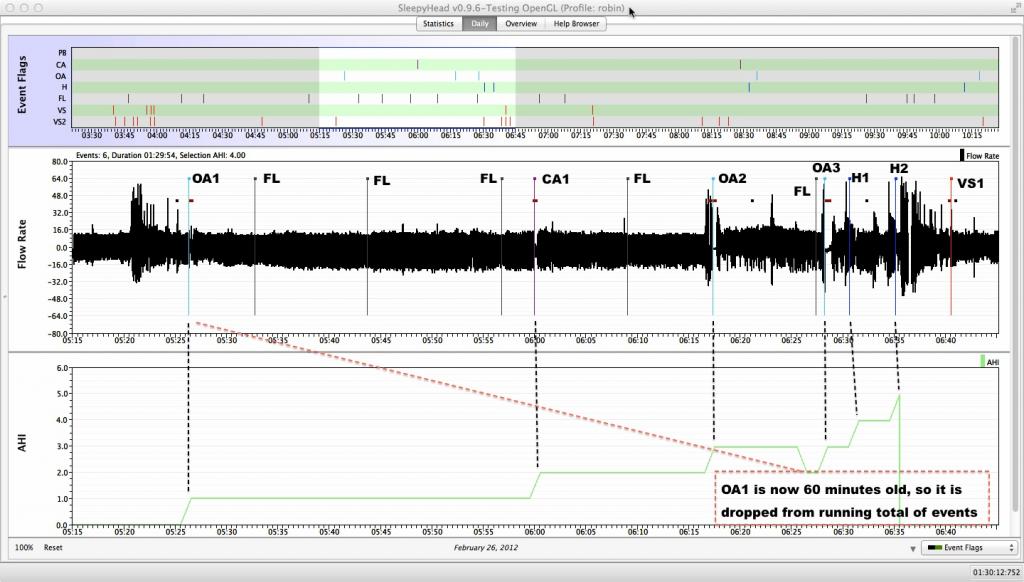
At this level of zooming, SleepyHead does not label the events; and hence each of the events have been manually labelled in this example, including flow limitations and the vibratory snore at the end of this window.
This particular hump in the AHI graph starts with OA1 at 5:26:21 with OA1, the first event recorded since the patient turned her BiPAP off and back on at 4:45. You'll notice that the AHI graph goes from 0 to 1 at this time. When CA1 is recorded at 6:00:00, the AHI graph bumps up to 2. When OA2 is scored at 6:17:21, the AHI climbs to 3.
At 6:26:21 the AHI graph goes DOWN from 3 to 2. The reason is that OA1 is now an hour old, and hence it is no longer included in the list "events that occurred less than an hour ago."
At 6:28:14, the machine records OA3, and so the AHI graph goes from 2 back up to 3. The machine records H1 at 6:30:39, and the AHI graph goes from 3 to 4 at this point. The machine records H2 at 6:35:09, and the AHI graph increases from 4 to 5. The patient wakes up shortly after H2 and turns her BiPAP OFF at 6:36:15. It's the turning the BiPAP off at 6:36:15 that causes the AHI graph to suddenly plummet from 5 to 0.
Note: Any time the CPAP machine is turned OFF and then back ON, the AHI graph is reset to 0 because a new session has started.
Note to only ResScan users: The AHI graph in ResScan resets to 0 at the top of every hour. Hence it is not going to look like the default SleepyHead AHI graph. If you want the SleepyHead AHI graph to look like ResScan's, you can use the "Zero Reset" option for the AHI/Hour graph in the SleepyHead Preferences. See 7. Important preferences settings for finding the "Zero Reset" option.
Basic data interpretation: Overview Data
Long term trends in the efficacy data are important for many reasons. One of the most important is that we all have the occasional bad night where the AHI is much higher than normal or the leaks are awful. Occasional bad nights do not indicate that there's something wrong with the way the CPAP therapy is going. (Although a really awful night for leaks might indicate it's time to replace those nasal pillows or to check whether the mask was put together correctly). Since sleep doctors meet with many patients each month, they tend to focus almost exclusively on the long term data---a small number of well-understood summary numbers and graphs are easier to review than massive amounts of daily data.
Overview data
The Overview data is a graphical representation of the highlights of the Detailed Daily data over a range of days (or months or years). Each of the graphs is either a bar graph or a line graph with one entry for each day's data. The following screen shot shows three of the more useful Overview data graphs from a sample patient:

The AHI graph
The bar for each day's AHI data is split into three colors; the relative sizes of each bar reveal the relative number of events. Bars that are
- mostly dark blue (like most of hubby's) indicate the user had more Hs scored than other events,
- mostly light blue indicate the user had more OAs scored than other events, and
- mostly purple indicate the user had more CAs scored than other events.
Looking at the data as a whole, we see that it took this patient about three weeks to really settle into CPAP and have the AHI come down to what's now his normal range. It's also interesting to note the spike in AHI on June 12. This particular patient had a bicycle accident on that day and got scrapped up pretty good, with a broken toe and a significant lacerations on his right ankle and shoulder. He was in pain that night, which is likely related to the higher AHI.
The Usage Compliance Overview
The usage graph is often mentioned, but it can be seen from the number at the top left of the graph that the patient is averaging 6:57 hours of mask time and that he's only had two days with really significant problems keeping the mask on. (One of those nights was during an overnight driving event where the patient didn't get to bed until 7:00 a.m.; the other was another cross country drive where he got to bed around 3:00 a.m.). The user is "compliant" by using the XPAP for more than 4-hours/day for at least 21 of 30 days, or 70% of days in a month.
Session Times Overview
The Session Times graph give a good overview of sleep patterns. If you sleep well, this graph probably won't be of much interest. If you have problems with insomnia or circadian rhythm problems, looking at the patterns in this graph may go a long way towards explaining why you may not be feeling much better even with CPAP: CPAP fixes OSA, but it does not fix bad sleep that are caused by other things. In the patient’s Session Times data, it's easy to see that his wake up times are a bit more regular than his bedtimes. It's also easy to spot which nights he had trouble keeping the mask on.
Scrolling down we can see additional graphs. Three more graphs that are often useful are shown below:
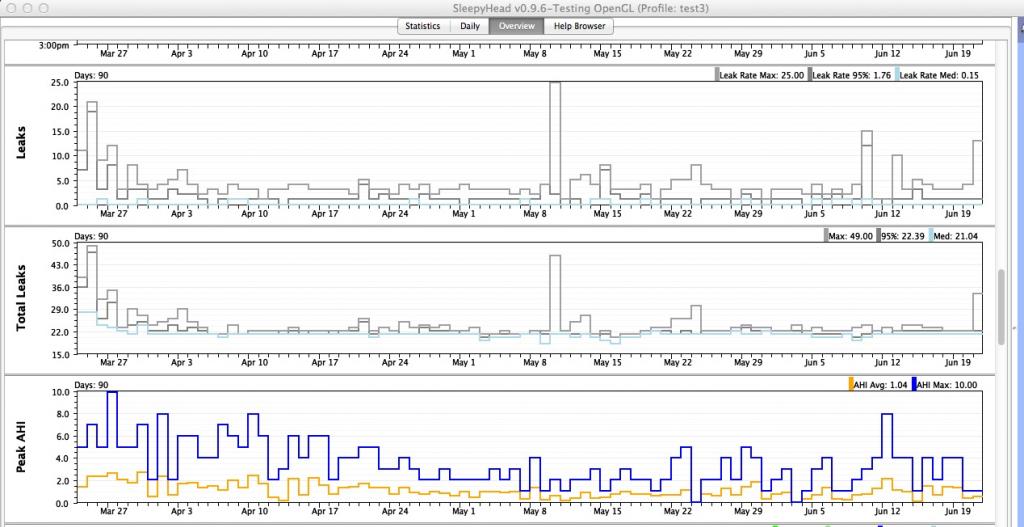
Leaks and Total Leak Overview
The Leaks and Total Leaks graphs show the maximum, 95%, and median Leaks and Total Leaks for each day. The 95% (or 90%) and median Leak graphs are are more important than the maximum values. The patient has had a few days where his 95% leak rate was pretty high, but not high enough to have had any leaks flagged as Large Leaks in his Daily Data.
Peak Hourly AHI Overview
The Peak AHI graph gives graphical information about the number of apneas and hypopneas recorded in any 60 minute period during the given night's data. The Maximum Peak AHI is the maximum number of events that occurred during any one hour of the given night; this is a crude measure of how bad the worst hour of the night was. The Maximum Peak AHI values are usually going to be quite a bit higher than the overall AHI for the night because for most of use, once we start CPAPing we have long period with no events and hopefully many hours where the hourly AHI is at or close to 0. This graph can provide insight whether apnea tend to be clustered, or spread out through the night. Clustered events often mean a positional apnea issue where the airway becomes obstructed as a result of the sleeper's posture (such as chin-tucking or poor head and neck alignment), rather than soft-tissue impingement on the pharynx in the airway.
Basic data interpretation: Statistics Data
This section will focus on how SleepyHead presents the long term summary data.
Organization of the Statistics Page
Below the SleepyHead header, the Statistics Page looks like this:
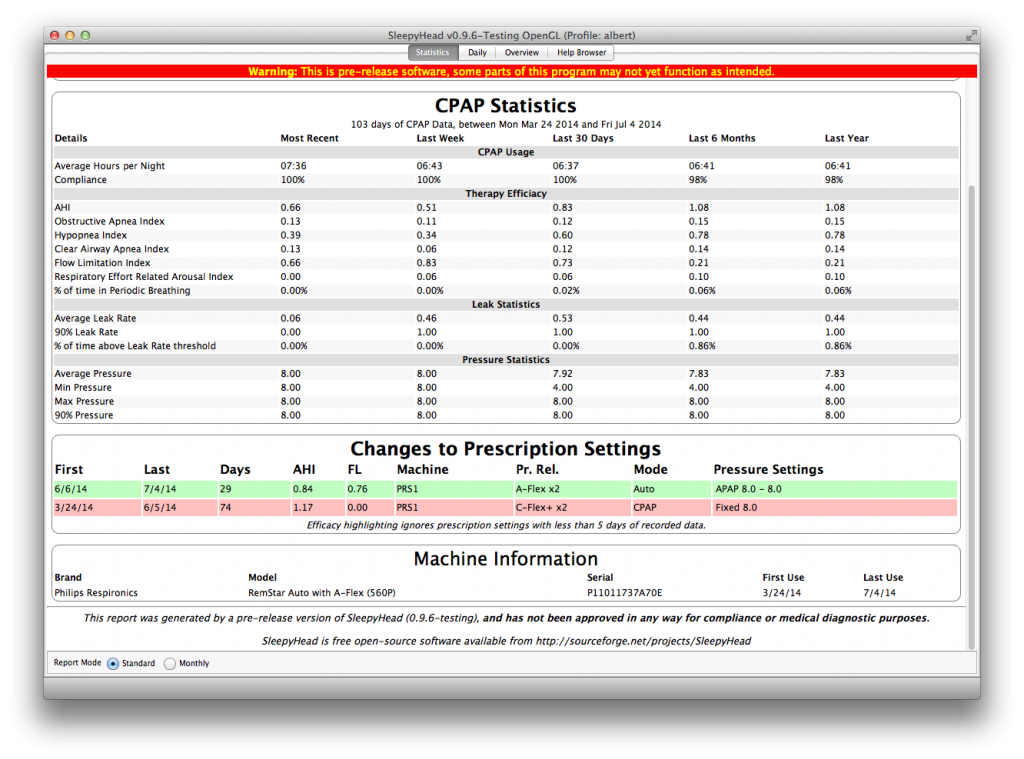
As you can see, the Statistics page has three major parts and two different "views". The parts are:
The CPAP Statistics. This chart has two distinct Report Modes. The Standard mode, which is shown here, is the default mode and it provides summary numbers for standard CPAP data reported for time ranging from the Most Recent (latest one-night) data to the data for the last year. The Monthly report gives summary numbers for each of the last 12 calendar months of data. Changes to Prescription Settings. This chart provides a list of all machine/prescription settings you have used. For a newbie, this chart should be relatively straightforward. Machine Information chart. This shows the make, model, and serial number for each CPAP machine that you've used with SleepyHead, as well as the first and last dates of usage.
The idea behind the Statistics Page is to provide a quick numerical view of the most important numbers from the efficacy data. This is the data that most Durable Medical Equipment (DME) suppliers print out from the proprietary software if the sleep doctor or insurance company wants more than just usage data. The organization of the summary data in the proprietary software varies from brand to brand, and we won't look at how the proprietary software organizes this data.
A detailed look at the CPAP Statistics
Here is our sample patient's CPAP Statistics chart:
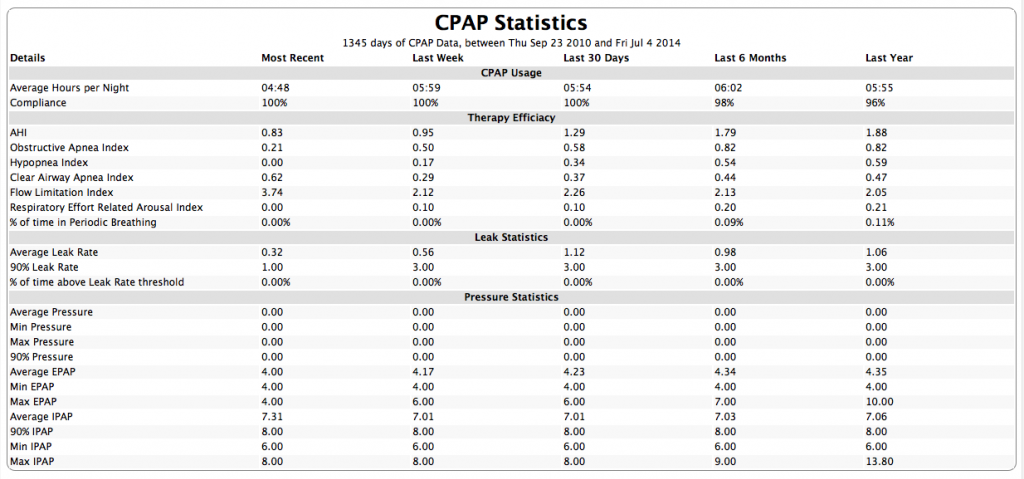
You will notice that the total number of days of CPAP data is listed immediately under the header CPAP Statistics. CPAP data includes data from any kind of CPAP machine that you have imported into the SleepyHead profile you are using. The dates of the range of data is also listed.
It's important to note that:
- Until you have more than 7 days of data the numbers in all columns except Most Recent will be the same
- Until you have more than 30 days of data the numbers in all columns except Most Recent and Last Week will be the same
- Until you have more than 6 months of data the numbers in the Last 6 months and Last year columns will be the same.
As you accumulate more and more data, you will start to notice that the numbers in the Last 6 months and Last year do not change very much from day to day.
The data in the CPAP Statistics is gathered in sections. We'll examine each of them in turn.
CPAP Usage data
The first two lines concern usage or compliance data:
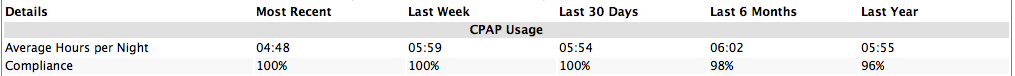
The numbers for Average hours per night is a simple average: Add up the usage for each night in the time period and divide by the number of days in the time period. We can see that the patient didn't get much sleep last night (July 4) and that she is averaging about 6 hours of mask time (and bed time) over the last year. There's a bit of variation between the 7-day, 30-day, 6-month, and 1-year figures, but the variation is not significant.
SleepyHead defines Compliance for a given night as "usage is at least four hours". The line for defining Compliance can be set in the SleepyHead preferences if desired. The percentage in the Compliance column is simply the percentage of days in the time period where the usage was at least four hours. The fact that the patient's 1-year compliance is listed as 96% means that the patient used her CPAP for at least 4 hours on roughly 350 or 351 days. (Both 350/365 and 351/365 round to 0.96). Of the 15 days where she was not compliant, most of them are nights where she got less than 4 hours of sleep. Notably, however, two nights were sleep tests performed during the past summer.
Therapy Efficacy data
The Therapy Efficacy data are the numbers that measure the overall effectiveness of your CPAP therapy. The whole point of CPAPing is to get and keep the AHI below 5.0 long term while also having the leaks under control and getting enough sleep to feel well in the daytime. Here are one patient's Therapy Efficacy data:
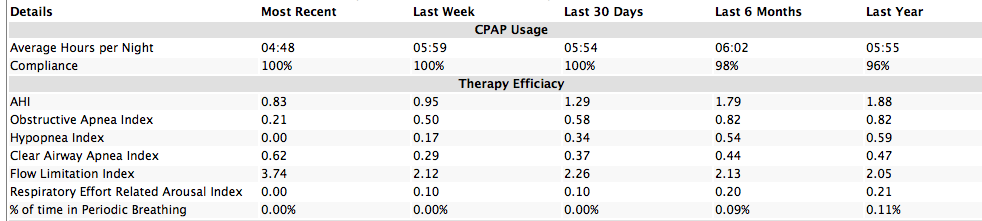
The indices in this list are the same as those listed on the Left Side Bar in the Daily Data. Exactly which indices will be listed here depends on the machine you are using:
- Philips Respironics System One users will see everything on this list.
- ResMed S9 users will see the AHI, Obstructive Apnea Index (OAI), the Hypopnea Index (HI), and Central Apnea Index (CAI).
- DeVilbiss IntelliPAP users will see the AHI, Apnea Index (AI), NonResponding Apnea Index (NRAI), and the Hypopnea Index (HI).
- Fisher & Paykel Icon users will see the AHI, Apnea Index (AI), and Hypopnea Index (HI).
The long term indices are computed in the same way the nightly indices are computed: SleepyHead counts the number of events recorded during the time frame for the index and divides that by the total run time for the time frame. In other words the long term indices are long term averages.
As an example: The patient's 6th month AHI = 1.79. This means that:
- (total number of OAs + Hs + CAs in the last six months)/(total run time in last 6 months) = 1.79
In other words, in the last 6 months, she had an average of 1.79 events each hour of sleeping with the machine. Some hours she had a lot more than that; other hours she had no events. But the expected number of events per hour of sleep would be 1-2 events each hour.
All the other indices are computed the same way and have the same meaning.
When we look at the numbers in aggregate, we can see some interesting things about this patient's data:
- Her Last Week numbers are quite a bit better than her 6-month and 1-year numbers. That means that her OSA has been better controlled this week than it has on average for the last 6 months. Her AHI numbers tend to be somewhat cyclic each month, and this week seems to have been a "good" week.
- The Last Month data is a bit better than the 6-month and 1-year data. So the last month has been a pretty good one in terms of CPAP therapy. SleepyHead data cannot provide an explanation of why it's better. However this patient is through her spring allergy season and the summer allergies have not been that bad this year. That may be a partial explanation for why the 30-day numbers are a bit better than the 6-month and 1-year numbers. More than likely her 30-day AHI will go back up once Ragweed starts to pollinate in the fall.
- The Last 6 month numbers are a tiny bit better than the Last year. The difference is not statistically significant. And taken together, the 6-month and 1-year numbers say that the machine is doing its job of preventing most of her apneas and hypopneas from happening. A long term AHI < 2.0 is quite good.
Leak Statistics
The Leak Statistics are based on the SleepyHead Leak data. SleepyHead uses Leak to represent the excess or unintentional leak rate. In other words, for machines that record Total Leak Rate data, it's important to understand that
- Leak Rate = Total Leak Rate - Intentional Leak Rate
SleepyHead uses a statistical analysis to estimate the intentional leak rate from the Total Leak Rate data and uses that to compute the Leak Rate. For more details about how SleepyHead handles Leak Rate and Total Leak Rate data see 8. Leaks.
The patient's summary Leak Statistics data looks like this:
NOTE: We've changed the patient's "top percentile" calculations to the 90% instead of the 95% because Encore reports 90% figures instead of 95%. Most SleepyHead users will see 95% numbers where this patient's data shows 90% numbers.
The average and 90% leak rates must be interpreted in terms of the statistical meanings of the words average and 90% (90th percentile) of a data set. For those who do not remember any about averages or percentiles, you may wish to read Average, Median, 95% numbers: A guide to those who don't remember their introductory stats.
We'll start with the 90% (or 95%) leak rates because they are actually easier to understand in terms of CPAP therapy.
The 90% and 95% leak rates are the 90th and 95th percentiles for the entire set of leak data for the given time frame. We can informally think about the computation needed to find the Last Week 90% leak rate as follows: Loosely speaking, the CPAP machine has sampled the leak rate a finite number of times in the last 7 days. So for the 7-day 90% leak rate, we can informally think of lining up all the sample leak data points for the last 7 days in increasing order. If there are 10000 sample data points on our list, we find the 90% by finding the 9000th number on the list because .90*10000 = 9000. The 95% leak rate would be the 9500th number on our list.
The 90% leak rates for 30-day, 6-month, and 1-year are found the same way: We line up all the data points for leak rate for the entire time period in increasing order. If there are n points on the entire list, we first find the integer k that is equal to or just barely bigger than 0.9*n and then we find the kth number on the list.
The meaning of the long term 90% leak rate is the same as the meaning of the daily 90% leak rate in the Detailed Daily data. The fact that the patient's 90% 6-month leak rate equals 3.0 means that for 90% of the time the patient's BiPAP has been on in the last 6 months, the unintentional leak rate has been AT or LESS than 3.0 L/min. We can also say that the patient's unintentional leak rate was ABOVE 3.0 for no more than 10% of the time her machine was running in the last 6 months. Which means that long term, she has no serious leak problems to worry about.
The average leak rate for a given time frame is just the (weighted) average for all the leak data in that time frame. In other words to compute the 7 day average leak rate, we look at all the leak rate data for the last 7 days as one data set and find the (weighted) average for the large data set. Loosely speaking, the CPAP machine has sampled the leak rate some very large, but finite number of times in the last 7 days. You add up all the "leak rate data points for the last 7 days" and divide by the total number of data points in the 7 days and you get the weighted average leak rate for the last 7 days.
The average leak rate for the last 30 days, last 6 months, and last year is computed the same way: Informally, you add up all the sample leak rate data points for the last 30 days, 6 months, or year (respectively) and divide by the total number of data points for the same period of time.
GEEK ALERT Skip the following paragraph if your eyes are starting to glaze over because you don't like dealing with statistics.
Understanding the long term average leak rate numbers is a bit more difficult simply because average leak rates do not have a simple "time" interpretation. Technically speaking, the leak curve is a continuous graph for each night. For the 7-day average leak rate, we string all seven of the leak curves together to get one very long curve that traps a finite amount of area between it and the horizontal axes for the graph. The 7-day average value for the leak rate would be the area under the 7-day leak curve divided by the total time the machine was running for the last 7 days. In other words, the 7-day average leak rate is just the average height of the leak curve over the course of the last 7 nights. (The idea is that the area under the curve really can just be thought of as the sum of the data points and the length of time is then just the number of data points.)
Note: Because of the way weighted averages are computed, we cannot conclude anything about how long the leak rate was AT or BELOW the 7-day, 30-day, 6-month, or 1-year average leak rates.
Pressure Statistics
The Pressure Statistics are not very interesting if you are using a fixed pressure CPAP machine; your max pressure and 90% or 95% pressure levels should equal your pressure setting. Your minimum pressure level and your average pressure level will be less than your pressure setting if you use the Ramp feature. The minimum pressure level will most likely be the starting Ramp pressure.
The Pressure Statistics are more interesting if you are using an Auto CPAP in Auto mode.
A sample patient's summary Pressure Statistics data looks like this:
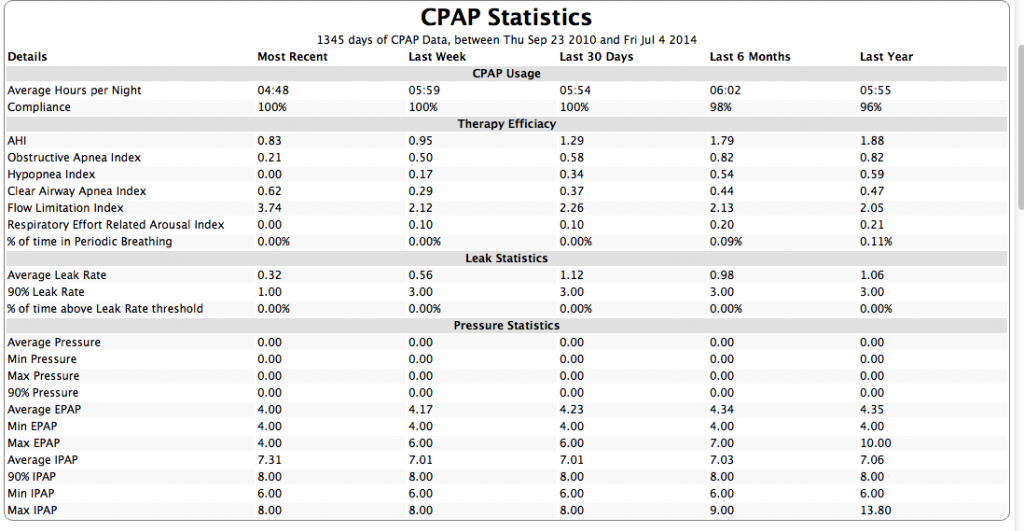
Two things need to be pointed out about this patient's Pressure data:
- Most people will have either "Pressure" data and no IPAP/EPAP data OR they'll have IPAP/EPAP data and no "Pressure" data. It's not certain as to why this patient has both. It could be a SleepyHead bug.
- We've changed this patient's "top percentile" calculations to the 90% instead of the 95% because Encore reports 90% figures instead of 95%. Most SleepyHead users will see 95% numbers where this patient's data shows 90% numbers
Several things should be pointed out about pressure data:
- Users of DeVilbiss IntelliPAP CPAP/APAPs, Fisher & Paykel Icon CPAP/APAPs, and Philips Respironics System One CPAP/APAPs will have Pressure data.
- Bi-level users will have IPAP/EPAP data regardless of the brand of machine.
- ResMed S9 CPAP/APAP users who use EPR will have IPAP/EPAP data because these machines act very similar to bi-levels. The IPAP data is the pressure level data; the EPAP data is the pressure level - EPR setting. In other words, if the pressure is 8 and EPR = 2, the IPAP = 8 and the EPAP = 6 = 8 - 2.
- If you use a Ramp, the Ramp pressures ARE used in the statistical computations. The min pressure, min IPAP, and min EPAP pressure numbers will typically be those used at the start of your ramp.
- The meaning of 90%, 95%, and average pressure and IPAP numbers are similar to the meanings of 90%, 95%, and average leak rates.
- The minimum and maximum pressure (IPAP/EPAP) numbers are true minimums and maximums. In other words, the 6-month min pressure number is the lowest pressure that's been recorded in the last 6 months; the 1-year maximum IPAP is the highest IPAP pressure that's been recorded in the last year.
Bugs in the CPAP Statistics data
There are some bugs in the CPAP Statistics numbers. So if a number obviously does not make sense, its best to disregard it.
Important preferences settings
When you select Preferences off the appropriate menu, a Preferences panel will come up. Regardless of whether you are using a Mac or a Windows computer, the Preferences panel will look the same. The default starting place in the Preferences panel is the Import pane.
The Import panel
The Import tab of the Preferences panel looks like this:

While looking at the Import tab of the Preferences panel, there are only two settings for a newbie to really worry about:
- Day time split. If you work shifts or often sleep past noon, changing this allows all your sleep data for one "night" to appear on the same day instead of being split across two days. NOTE: Day time split is NOT available after you import data from an S9 into SleepyHead. This choice was intentional since disabling Day time split is needed to make it possible for SleepyHead to get at the S9's summary data.
- Create SD card backups during Import. As the parenthetical note says, making sure this is checked is pretty critical for ResMed S9 and FP Icon users since those machines overwrite the detailed data on the SD card on a regular basis. Checking this will make it easier to reimport the data if it becomes necessary.
All other settings on this page can be left at the default settings until you're more comfortable with SleepyHead. (NOTE: this patient's settings are NOT the default settings.)
The CPAP panel
The CPAP tab of the Preferences panel looks like this:
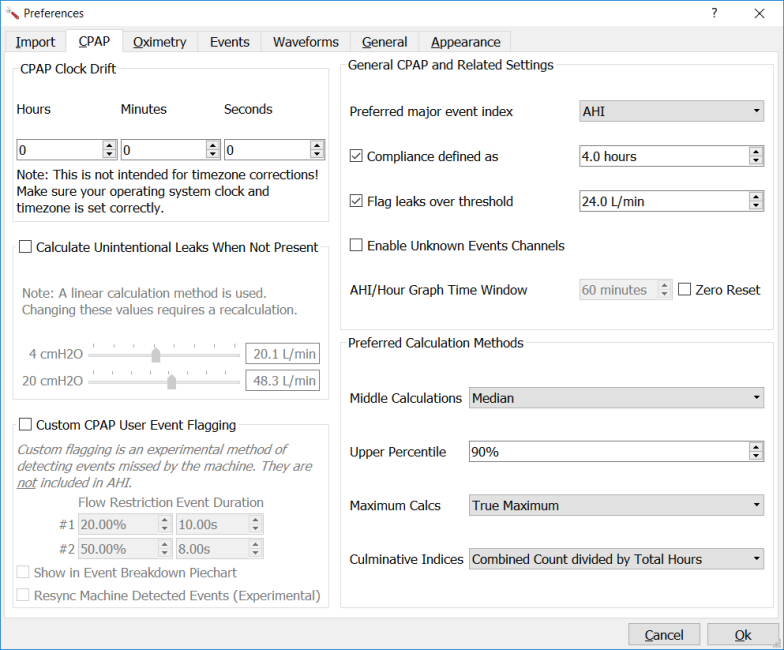
The default values have been edited on the patient's profile. Things of note for a newbie:
CPAP clock drift
Clock Drift should be left at 0 hours, minutes and seconds unless you know your CPAP clock is off and you can't change the CPAP's internal clock. With Resmed models you can set the clock in CPAP settings. Philips Respironics owners cannot access the clock, and may need to offset time drift. The best way to do this is to record your start-time, and reset the clock drift the next day using the CPAP Clock Drift. Time offsets may be positive (advance time), or negative (move time back). For example, if your start time is 10:00 PM and the Sleepyhead charts show a starting time of 08:15, you need to move the time ahead +01:45. If the starting time on the charts shows 00:10:00, the time would be moved back -01:50:00.
Show Leak Redline
The default is to have this checked and the default value for the Redline is the ResMed value of 24 L/min. If you are using a ResMed S9 or S10, it's strongly recommended that you make sure Show Leak Redline is checked. If you are using a different machine, this may be a useful option for you, but you will need to change the value for the Redline to reflect. See A detailed look at the Show Leak Redline option
- Show compliance affects how low usage days show up in the Overview data and the compliance data in the Statistics page. The default line is 4 hours for obvious reasons. It's suggested that you leave this alone. Most insurance defines "Compliance" as greater than 4-hours of therapy in any 24-hour period, for 70% of any month (21 of 30 days).
- Custom User Event Flagging. It's recommended that most users leave this unchecked. It can be useful if you have a lot of "almost" apneas or "almost" hypopneas showing up in your detailed data, but it really is an advanced feature.
- AHI/Hour Graph Settings. The default is to have the box by Zero Reset unchecked. Leaving the box unchecked tells the AHI/hour graph to keep a running total of the number of events (OAs + CAs + Hs) that have happened in the last 60 minutes. To make the AHI/hour graph behave like the ResScan AHI/Hour graph, you need to check the Zero Reset box; then the AHI count is set back to 0 at the top of every hour.
A detailed look at the Show Leak Redline option
The default is to have this checked and the default value for the Redline is the ResMed value of 24 L/min. This is a NEW feature in SleepyHead 0.9.6. Since our sample patient uses a Philips Respironics System One and she pretty much understands her leaks, she has unchecked the Redline so she doesn't get one in her daily leak graphs. If you want a line for helping you spot Large Leaks and you are NOT using a ResMed S9 machine, the first thing you will need to do is figure out whether your machine's manufacturer has an official definition of "Large Leak" or not. Here is some information on that:
- ResMed S9 and Airsense 10. You should use the default Redline setting of 24 L/min, and and you want to keep the Leaks graph under this line.
- Fisher & Paykel Icon. The Fisher & Paykel Icon reports TOTAL leaks and the Fisher & Paykel Icon definition for Large Leak is a TOTAL leak rate that is above 60 L/min. You should set the Redline at 60 L/min and you want to keep your TOTAL leaks under a Redline drawn at 60 L/min.
- Devilbiss IntelliPAP Auto. The Devilbiss IntelliPAP reports Total leaks and the Devilbiss definition of Large Leak is a TOTAL leak rate that is above 95 L/min. You should set the Redline at 95 L/min and you want to keep your TOTAL leaks under a Redline drawn at 95 L/min.
- Philips Respironics System One and Dreamstation. The Philips Respironics machines report TOTAL leak, but Philips Respironics never tells us what the official definition of a Large Leak. SleepyHead 0.9.6 now flags the official Encore Large Leaks as gray bars over the Flow Rate graph. So if you get a lot of large leaks, you can use that data to help you decide where to draw a Large leak line. But until you get some data, here's a staring place to make some guesses about where to draw the Redline that are based on looking at a lot of Encore data from a lot of Philips Respironics users over the years:
- Older Series 50 System One machines. If you are using a pressure setting that is higher than 8-10cm, Encore usually does not flag Large Leaks until the Total Leak rate is up around 90-100 L/min. If you are using very low pressures (4-8cm), Encore may start flagging large leaks at around 60 L/min. So start by selecting a Redline of 90 L/min if you are using pressures above 8 cm and a Redline of 60 L/min if you are using pressures below 8 cm. Adjust if you see Gray Large Leak bars in your actual data.
- Newer Series 60 System One and Dreamstation machines. If you are using a pressure setting that is higher than 8-10cm, the Encore software usually does not flag Large Leaks until the Total Leak rate is up around 80 L/min. If you are using very low pressures (4-8cm), Encore may start flagging large leaks at around 50 L/min. So start by selecting a Redline of 80 L/min if you are using pressures above 8 cm and a Redline of 50 L/min if you are using pressures below 8 cm. Adjust if you see Gray Large Leak bars in your actual data.
The Graphs panel
The Graphs tab of the Preferences panel contains a list of all potential graphs that SleepyHead can draw along with a minimum and maximum value for each graph. The panel looks like this:
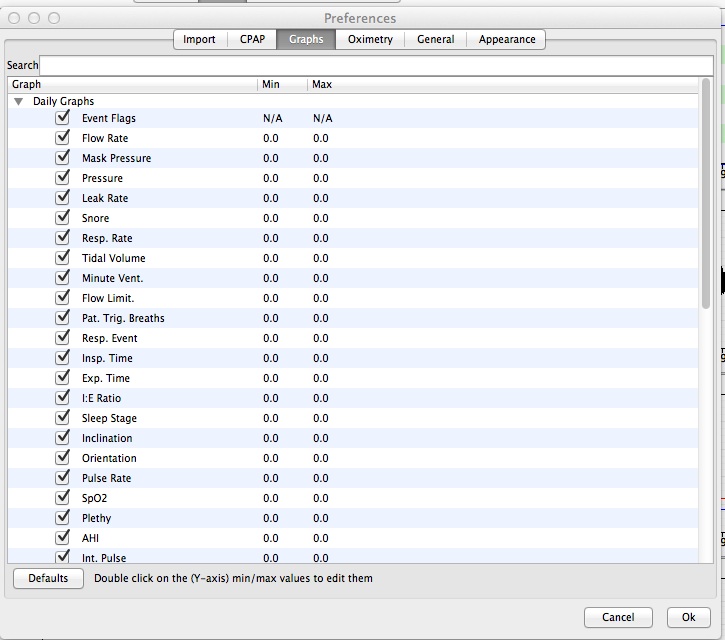
Note that there are going to be graphs on this list that do NOT show up in your particular data; that's because this is a master list of all the graphs for all the machines that SleepyHead supports. If your machine does not record a particular kind of data, you won't have that graph show up in the daily data, even though it will be listed here.
The "default" values where both the min and max values are set to 0.0 allows SleepyHead to choose the values for the vertical scale of the graphs. Most of the time those default values are just fine. However, sometimes the the default values compress the data too much vertically and that can leave a lot of "unused white space" in the graphs. If you want to change a graph's values, double click on the particular value you want changed, and you'll be able to edit it:
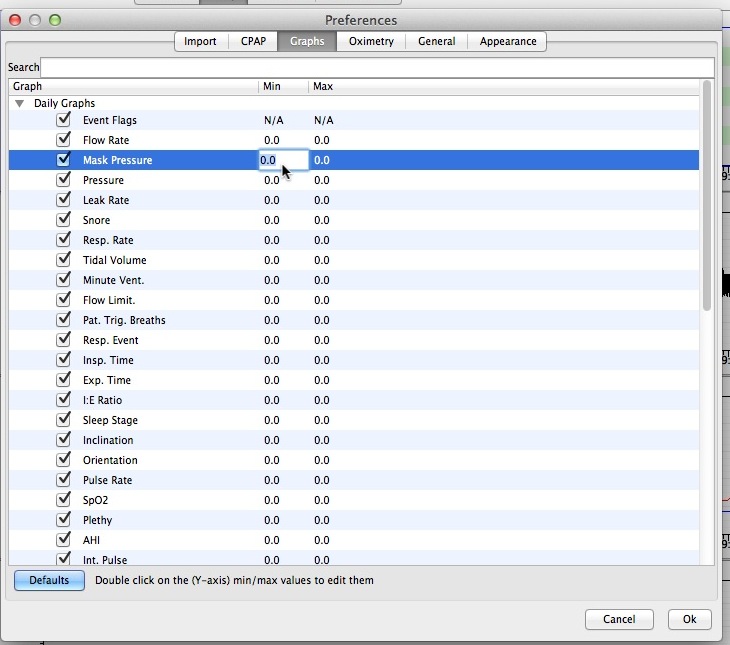
SleepyHead should save your graph settings after you've changed them, so you really only need to edit the y-values for the graphs once.
The values that make sense for our sample patient's data are probably NOT a good starting point for most people since she is a petite 5'1" female who weighs about 110 lbs. That said, here's what the value she typically uses for her graphs look like:
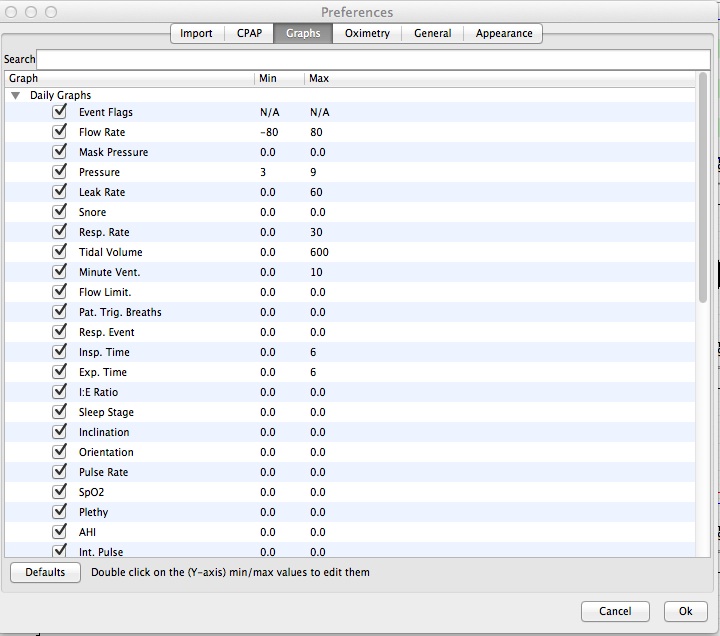
The General panel
The General tab of the Preferences panel looks like this:
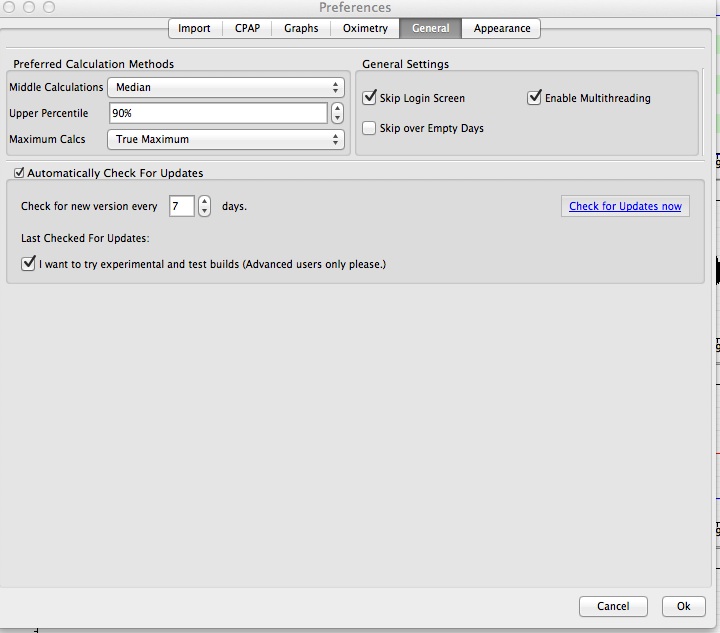
The patient here has edited some of her settings. For a newbie, the default settings are fine.
The default Upper Percentile Calculation is 95% (the ResMed number), but the sample patient prefers to use the 90% numbers, since they agree with Encore, the official manufacturer software for her machine.
Median is a better choice for the "middle" calculation than either "Average" or "Weighted Average" from a mathematician’s perspective. The numerical average and weighted average are not a meaningful as Median is. The Median is the "middle" point of the data---50% of the data lies AT or BELOW the median and 50% of the data lies AT or ABOVE the median. Both the Average and Weighted Average can be (seriously) skewed by even a tiny bit of outlier data.
The default for "Skip over Empty Days" is to have the box checked; This patient wants to be reminded that there's no data for a particular day, so she unchecked that box.
The default for "I want to try experimental and test builds" is to have the box unchecked. For a new user that's the right choice.
The Appearance panel
The Appearance tab of the Preferences panel looks like this:
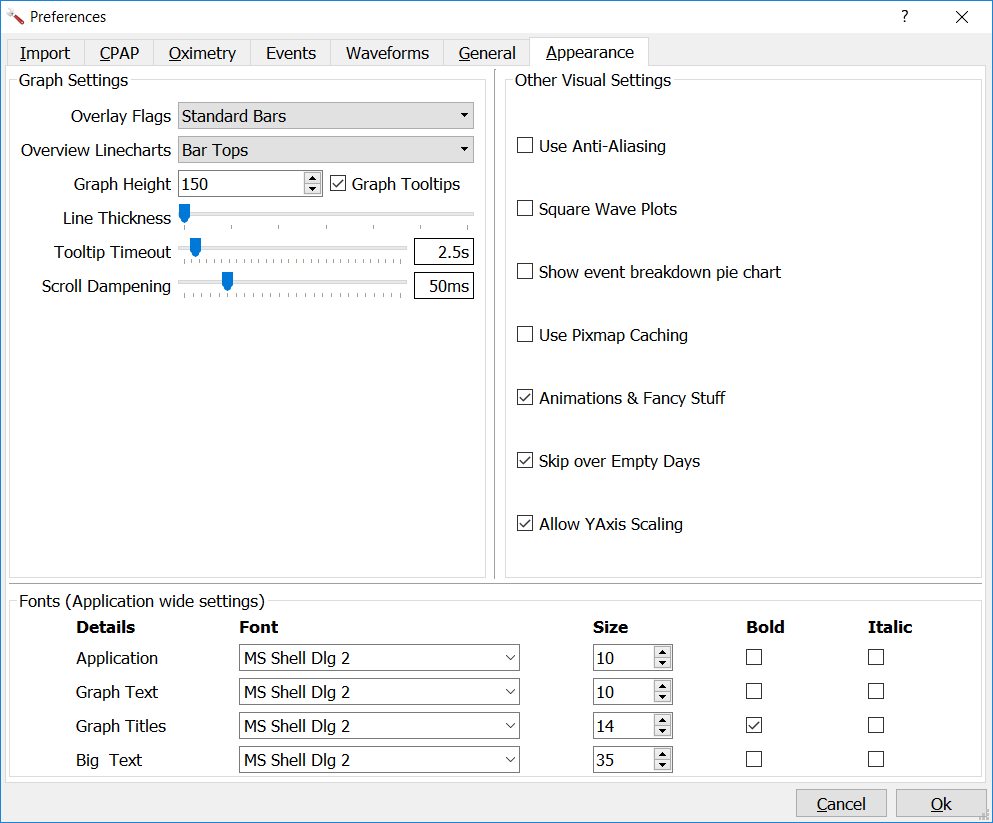
Some of these values have been edited. By default, the default values for the check boxes are:
- Use Anti-Aliasing is turned OFF
- Use Square Wave Plots is turned OFF
- Show event break down pie chart is turned ON
- Use Pixmap Caching is turned ON
- Animations & Fancy Stuff is turned ON
- Allow Yaxis scaling is turned ON
For most users, the default settings can be left alone, with the following possible exceptions:
- Show event breakdown pie chart should be turned off for the purpose of posting images on the forum. This allows more valuable information to be seen.
- Use Pixmap Caching. By default, this is turned on; It's recommended that you turn "Use Pixmap Caching" off by deselecting the box. Pixmap Caching can make some of the graphics stuff go faster, but it can also cause problems, particularly if your graphics card is not standard. Most patients routinely turn Pixmap Caching off by unchecking the box because there is no noticeable speed up when Pixmap Caching is turned ON. Some have reported bizarre problems with the graphs when Pixmap Caching is turned ON that seems to go away when Pixmap Caching is turned off.
Leaks
All masks leak-- they all have an intentional leak rate built into their design to prevent re-breathing of CO2. This intentional, expected leak rate varies with the pressure level: As the pressure goes up, so does the intentional leak rate for the mask. The leak rate also varies from mask to mask. Typically full face masks have larger intentional leak rates than nasal masks or nasal pillows masks when used at the same pressure.
Excessive leaking is when the total leak rate detected by the machine is larger than the intentional leak rate for the mask. Excessive leaks are an ongoing issue for some CPAP users. A full understanding of the leak information reported by SleepyHead requires that you understand what kind of leaks your machine reports and how your machine's manufacturer defines Large Leak.
NOTE and CAUTION: When looking at Leak/Total Leak lines in both your data and others, you must take into consideration all of the following:
- Does the CPAP report Total Leak Rate or Excessive Leak Rate?
- What is the definition of Large Leak for the particular machine?
- If we're looking at Total Leak, what is the expected leak for the mask at the given pressure(s)?
- What is the vertical scale of the Leak/Total Leak graph?
Difference between Total Leak Rate and Leak Rate
All machines other than ResMed record and report the Total Leak Rate. Total Leak Rate includes both the intentional leak rate built into your mask to prevent re-breathing of CO2 AND any excessive (bad) leaks. In other words:
- (Total) Leak = Intentional Leak + Excessive Leak
ResMed machines record and report only the Excessive Leak. The S9 takes the raw (total) leak data and the mask setting and uses that to record the Excessive Leak data. The raw Total Leak Rate data is not recorded to the SD card or the machine's internal memory.
SleepyHead uses Total Leak Rate to refer to the leak data recorded by Philips Respironics, Fisher & Paykel, and DeVilbiss machines; the SleepyHead Total Leak Rate includes both the intentional leak rate and the excessive leak rate. SleepyHead uses Leak Rate to refer to only the excessive leak rate. It's important to remember the following things about the SleepyHead Total Leak/Leak Rate data:
- ResMed users will only have ONE leak line and it is Leak Rate.
- Philips Respironics, Fisher & Paykel, and DeVilbiss users will have TWO leak lines: One for Total Leak Rate and one for Leak Rate.
- The Leak Rate for Philips Respironics, Fisher & Paykel, and DeVilbiss users is calculated by SleepyHead from the data recorded by the machine. SleepyHead uses a statistical analysis of the Total Leak Rate data to determine an estimate for excessive leak rate and reports that estimate as Leak Rate. If you are using a bi-level device or if you are using an APAP with a wide range of pressures, it is possible that the estimated excessive leak rate may not be accurate; in that case you are better off looking at the Total Leak Rate data and using it to determine how good or bad your leaks are.
Both Total Leak Rate and (excessive) Leak Rate are reported in terms of Liters per minute (L/min).
A Total Leak Rate of 25 L/min means that on average, the semi-closed pressurized system comprising your upper airway, the mask, the hose, and the blower is losing approximately 25 Liters of air for each minute of run time. The blower has to add at least 25 Liters of air to the system each minute in order to maintain the desired pressure.
An (excessive) Leak Rate of 25 L/min means that the semi-closed system is losing 25 L/min of air ABOVE and BEYOND the expected leak rate for the mask. If the mask has an expected leak rate of 30 L/min and the (excessive) Leak Rate is 25 L/min, then the Total Leak rate is 55 L/min. The blower has to add at least 55 Liters of air to the system each minute in order to maintain the desired pressure.
Definition of Large Leak
Modern CPAP machines are designed to gracefully cope with a certain amount of excessive leak by blowing additional air into the semi-closed system in order to preserve the desired pressure setting. But even the best of machines cannot accommodate really large amounts of excess leak.
When the excess leaking reaches the point where the machine's manufacturers are concerned that the machine will not be able to properly maintain the therapeutic pressure setting, the leak is defined to be a Large Leak. Different manufacturers define and flag Large Leaks in different ways. Typically, however, Large Leaks are defined in terms of the Total Leak Rate for machines that report Total Leak Rate. ResMed, of course, must define Large Leak in terms of the (excessive) Leak Rate that is reported by their machines.
- ResMed S9: When the Leak Rate is AT or ABOVE 24 L/min, it is a Large Leak.
(Source: ResScan Interpretation Guide)
In ResScan, Large Leaks are flagged by a Red Line drawn at 24 L/min in the (excessive) leak graphs. ResMed S9 users can use the Show Leak Redline option to draw a Red Line at 24 L/min in the Leak Rate graph in SleepyHead 0.9.6. (Earlier versions of SleepyHead do not have this option.)
- DeVilbiss IntelliPAP: When the Total Leak Rate is AT or ABOVE 95 L/min, it is a Large Leak.
(Source: CLINICAL OVERVIEW: DeVilbiss IntelliPAP® AutoAdjust)
In DeVilbiss's software, Large Leaks are flagged by a line drawn at 95 L/min in the (total) leak graphs. DeVilbiss IntelliPAP users can use the Show Leak Redline option to draw a Red Line at 95 L/min in the Leak Rate/Total Leak Rate graph in SleepyHead 0.9.6. (Earlier versions of SleepyHead do not have this option.)
- Fisher & Paykel Icon: When the Total Leak Rate is AT or ABOVE 60 L/min, it is a Large Leak.
(Source: F&P InfoSmart Spec Sheet)
In Fisher & Paykel's InfoSmart software, Large Leaks are flagged by a line drawn at 60 L/min in the (total) leak graphs. DeVilbiss IntelliPAP users can use the Show Leak Redline option to draw a Red Line at 60 L/min in the Leak Rate/Total Leak Rate graph in SleepyHead 0.9.6. (Earlier versions of SleepyHead do not have this option)
- Philips-Respironics System One: There is no official "line in the sand" for flagging a Large Leak.
(Source: Encore Report Guide) Lots of System One user data posted on the forum indicates the Large Leak line for Total Leak Rate depends on whether the machine is a Series 50 (older) System One or a Series 60 (newer) System One. Lots of user data posted on the forum also indicates that the Large Leak line depends on the pressure used: People using less than 10 cm of pressure see Large Leaks being flagged much earlier than people using pressures greater than 10 cm. Here are some general estimated guidelines for where the undefined Philips Respironics Large Leak line is located:
- Series 60 System One users may start to see Large Leaks being flagged when the Total Leak Rate reaches 60-70 L/min; if the prescribed pressure setting is below about 8cm, then Large Leaks may be flagged when the Total Leak Rate reaches 50-60 L/min in some circumstances.
- Series 50 System One users may start to see Large Leaks being flagged when the Total Leak Rate reaches 80-90 L/min; if the prescribed pressure setting is below about 8cm, then Large Leaks may be flagged when the Total Leak Rate reaches 60 L/min in some circumstances.
Official Large Leaks for Philips Respironics System One machines are very difficult to determine with great accuracy in versions of SleepyHead prior to 0.9.6. In version 0.9.6, the Encore-defined Large Leaks are flagged by gray bars in the Events table and as a gray background in the Flow Rate curve. The Official Large Leaks for a System One will NOT be flagged directly on the SleepyHead Leak/Total Leak graph.
If you want to add a Redline to your Leak/Total Leak graphs in SleepyHead, our advice is to look at your own Large Leak flags and figure out where they seem to start. If you don't seem to have very many Official Large Leak, then use the above guidelines as a decent enough starting guess for where your particular Redline should be drawn.
In order to adversely affect the efficacy of your CPAP therapy and the accuracy of the data recorded by your machine, leaks have to be both large enough and long enough. As we've just seen, "Large enough" is easily quantified by the manufacturers. But what is "long enough"?
ResMed is apparently the only major manufacturer that has a user-friendly tool for determining whether the official Large Leaks last long enough to compromise the CPAP therapy: The dreaded Mr. Red Frowny Face shows up on the short version of the Sleep Quality Report when Official (ResMed) Large Leaks make up at least 30% of the night.
Since the other manufacturers are "vague" when it comes to describing how long Large Leaks must last to adversely affect the CPAP therapy, we'll take that ResMed definition as a "working" definition:
- If you are in Official Large Leak territory for your machine for at least 30% of the night, then you KNOW you have a Large Leak problem that must be dealt with.
A lot of long-time CPAP users will say that the "30% time in Large Leak territory" is too generous and that Large Leaks will affect your therapy much sooner than that. So this may be a good rule of thumb for you to consider:
- If you are OFTEN in Official Large Leak territory for 15%-30% of the night, then you PROBABLY have a Large Leak problem that must be dealt with.
- If you are OFTEN in Official Large Leak territory for 10%-15% of the night, then you MAY have a Large Leak problem that must be dealt with.
- If you OFTEN have Official Large Leaks that last an hour or more, then you PROBABLY have a Large Leak problem that must be dealt with.
All that said: It's not uncommon for people to simply have a bad night for leaks every now and then. If your leaks are usually decent enough, it can be counter-productive to worry about eliminating the last of the leaks.
Perfect Leak/Total Lines
A perfect Leak/Total Line is a leak line with little or no unintentional leaks.
For ResMed users, that's easy to recognize: The Leak graph is a flat line at 0.0 L/min for all or almost all of the night. And any leaks that are present are way, way below the ResMed Redline of 24 L/min.
For all the rest of us, perfect leak lines are not quite so easy to recognize. We can use SleepyHead's estimated Leak graph (rather than the Total Leak graph), but that may not always be accurate, particularly if we're using a bi-level or an auto machine with a wide range of pressures.
To identify a perfect leak line from Total Leaks requires a bit of knowledge: We need to know the expected (intentional) leak rate for the mask. Once we know that, a perfect Total Leak line would be a flat or "fuzzy flat" line that is within a few L/min of the expected leak rate for the mask at the given pressure.
The expected rate depends on both the mask and the pressure. The owner's manual for your mask should have a table and/or graph that tells you what your mask's expected (intentional) leak. The chart below shows the design flow rate at different pressures for a variety of masks and mask types:
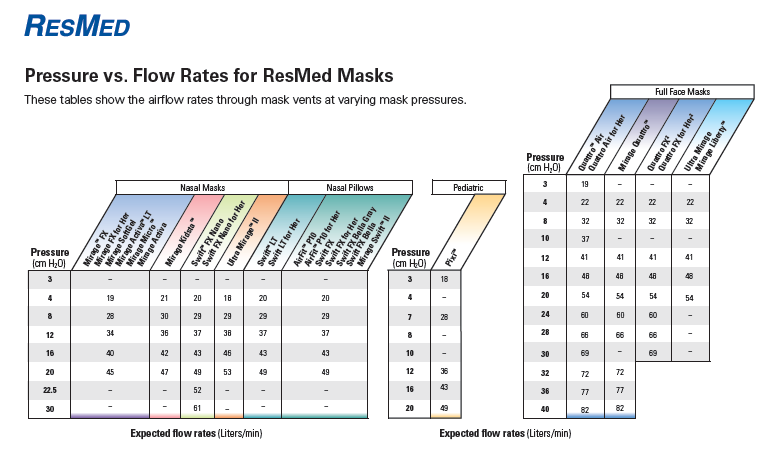
For the Swift FX mask, We interpret this chart as follows:
- If your pressure is set at 6cm, your expected leak rate is about 25 L/min.
- If your pressure is set at 9cm, your expected leak rate is about 30 L/min.
- If your pressure is set at 10cm, your expected leak rate is about 32 L/min.
- If your pressure is set at 14cm, your expected leak rate is about 40 L/min.
- If your pressure is set at 15cm, your expected leak rate is about 41 L/min.
- If your pressure is set at 18cm, your expected leak rate is about 48 L/min.
These numbers are not precise-- they typically include a +/- margin of error of about 5 L/min. But in an ideal world, you want your Total Leak graph to be pretty close to your expected leak rate.
Good and Decent Enough Leak/Total Leak lines
We'd all like a perfect leak line every night. But for most of us, that's not going to happen. Moreover, the battle to eliminate all excess leaks may cause more problems than it fixes. So when are leak lines "good enough" to not worry about it?
In general a Total Leak line will be mostly "fuzzy" flat and stay mostly around the intentional leak rate for your mask and pressure, but tends to have some visible periods of noticeably higher leaks, most of which stay well below the cut off for "Large Leaks" for the given machine. A few very short lived Large Leaks on an otherwise decent night are usually not something that you need to worry about. A Decent Enough Total Leak line has more obvious leaks than a Good one does, but line stays below the Large Leak line for at least 70-90% of the night. (There's some debate between CPAP users of just how long the Large Leaks need to last before they become problematic.)
For ResMed users or for folks who simply want to concentrate on the (excessive) Leak data, a Good Leak line will be "fuzzy" flat, stay mostly around 0.0 L/min, but tends to have some visible periods of noticeably higher leaks, most of which stay below 10-15 L/min. A Decent Enough Leak line has more obvious leaks than a "Good" one does, but line stays below 25-30* L/min for at least 80-90% of the night. (There's some debate between CPAP users of just how long the Large Leaks need to last before they become problematic).
- In general patients can trust the Total Leak data and the machine manufacturer's Large Leak definition more than eye-balling the (excessive) Leak graph in SleepyHead if one is indicating there's a Large Leak and the other is not. That means that users of IntelliPAP machines may have a bit higher "Leak" number than 24-30 L/min before it really counts as a Large Leak; on the other hand users of Icons with masks that have relatively high expected leaks may have Large Leaks where the (excessive) Leak graph is quite a bit lower than 24 L/min: If the expected leak rate of your graph is 45 L/min and you use an Icon, any excess Leak that is more than 15 L/min is likely be flagged as an Large Leak in the Fisher & Paykel software since the Total Leak will be AT or ABOVE 60 L/min, which is the Large Leak line for the Icon.
Here's an example of a "Decent Enough" leak line from our sample patient's own data:
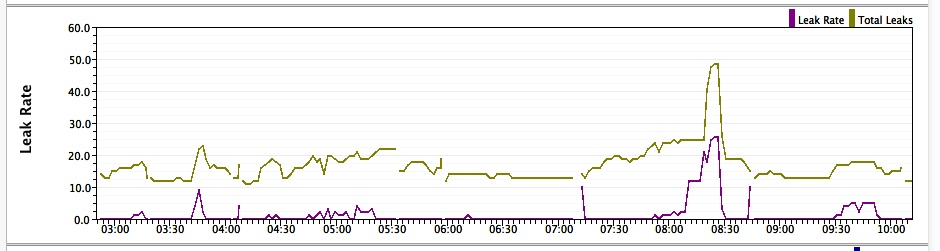
That large bump between 8:15 and 8:30 is a (relatively speaking) a very large leak for this patient; the Total Leak Rate is up close to 50 L/min, which is beginning to approach the boundary where her rare Official Large Leaks have been scored (about 55-60 L/min). But this rather large leak makes up only about 15 minutes out of 7 hours of run time; that's not enough time to really worry about.
The 90% or 95% Leak/Total Leak Rate from the Left Side bar may also useful for determining that your leaks are under control. Typically if the 90% or 95% Leak/Total Leak Rate is below the definition for Large Leak for your machine, the leaks are pretty much under control. On the night shown above, the patient's 90% Total Leak rate for this night was 22 L/min, which is right around her expected leak rate.
But it's also important to understand that if the 90% or 95% Leak/Total Leak Rate is just barely above the definition for Large Leak for your machine, your leaks might still be "decent enough". In this case you really do need to consider just how much time you spent in Large Leak territory: It's one thing if you are spending 15-20% of the night barely above the Large Leak line; it's another thing if you're spending 40-45% of the night AT or ABOVE the large leak line. And yet, the 90% (and 95%) Leak/Total Leak numbers can look the same for both situations.
Problematic, Bad, and Horrible Leak Lines
As with many other things concerning CPAP therapy, trending data in the Leak/Total Leak line is also important. If you're trying out a new mask and you're still working out how to fit the mask, you may have one or more nights of really bad Large Leaks. If your mask cushion is starting to wear out, the first sign might be a higher than normal leak line. If you wind up with a bad cold or the flu and you're seriously congested, you might be prone to doing more mouth breathing than normal and your leaks may be (much) higher than typical. So it's important to not over-react to one (or a few) bad nights with respect to leaks, particularly if there's an obvious explanation.
But some new CPAP users (and not so new CPAP users) have real problems getting excessive leaking under control. We now turn our attention to using the Leak/Total Leak line to identify when Large Leaks are long enough as well as large enough to compromise the efficacy of the CPAP therapy and the accuracy of the data.
There is some differences of opinion among long term CPAP users about how much time you have to spend in Large Leak territory before it becomes clear that you absolutely must do something about the leaks. Some people would say 10% of the night in Large Leak territory is too much; others would say 10% is ok, but 20% is not. Some of this comfort: If the Large Leaks are waking you up, they've got to be dealt with. If you're not feeling better in the daytime, the Large Leaks might be part (or all) of the problem. But if you're sleeping through the Large Leaks and you're feeling good in the daytime, it may not be all that important if you are in Large Leak territory 10-20% of the time on some nights.
But by the time Large Leaks make up 30% or more of the night, you have a problem. ResMed is explicit about this line; the other manufacturers are more vague.
And then there's also the issue of how long the longest of the Large Leak is: If you see 40+ minute long official Large Leaks on most of your nights, then that's likely a problem that you need to work on.
Here is an example of a Bad (excessive) ResMed S9 Leak Line shown in SleepyHead 0.9.3. We've added a red dashed line at the ResMed Redline at 24 L/min since it was not drawn by SleepyHead 0.9.3:
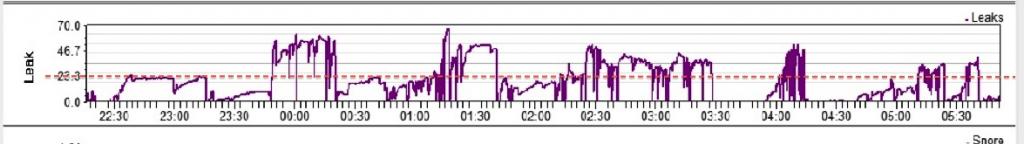
We can estimate the time over the Redline. (In SleepyHead 0.9.6, the percent of time over the Redline would be in the Statistical Data in the Left Side Bar). Our estimate is that the time where the Leak is above the ResMed RedLine of 24 L/min is between 180 and 200 minutes, or between 3 and 3.33 hours. The run time for the night is about 8 hours. So it looks like this person was in Large Leak territory for 37% of the night.
Most of the time when someone has serious Large Leak problems, the Leak/Total Leak line is problematic-to-horrible on a large percentage of nights. So the easiest way to tell that you've got a Large Leak problem is realize that you are often spending more than 30% of the night in Large Leak territory. Or you realize that you are often spending 10-30% of the night in Large Leak territory and you are not feeling as good as you should.
Mouth Breathing and Other Causes of Leaks
A lot of things can cause leaks of all sizes: Fiddling with the mask, jostling the mask to scratch your nose, jostling the mask while turning over in bed, mouth breathing, and facial relaxation (facial sagging) in deep sleep are all capable of causing both small and large leaks. Worn out mask cushions, incorrectly sized masks, overtightened mask straps, and masks that are incorrectly reassembled can also cause leaks. Another potential cause of leaks are pressure increases when using a CPAP in auto mode. Fitting a mask at low pressure tends to be easier than fitting a mask at higher pressures. And if you fit your mask at relatively low pressure, as the pressure increases, the pressure increase itself may cause the mask to lose its seal, and the result is an excessive leak.
Mouth leaks can be particularly problematic for nasal mask and nasal pillows users. Indeed new CPAP users using nasal masks and nasal pillows are often told by other CPAP users that they need to use a full face mask if there is any chance that they might be a mouth breather. And when a newbie posts pictures of problematic leak lines, the first thing that's often suggested is that the leaks are probably due to mouth breathing.
But a leak is a leak no matter where it is coming from, and the machine doesn't know where it is coming from. So how do we determine if a leak is a mouth breathing leak or just a typical mask leak caused by something else? Well, it's kind of difficult, but in general we look at the leak line on the graph. Short brief spiky leaks are very likely mask movement leaks... brief refitting or minor movement. Longer periods of spiky leaks may indicate that you were very restless and doing a lot of tossing and turning and repeatedly jostling the mask in the process. Mouth-breathing leaks tend to have a longer period of leak and often tend to sort of create a a mesa or plateau effect. But facial relaxation can also lead to longer periods of leak that look like mesas or plateaus.
In this example pulled from some old on-line ResMed materials, there are actually 3 periods of probable mouth leak but only the middle one went above 24 L/min:
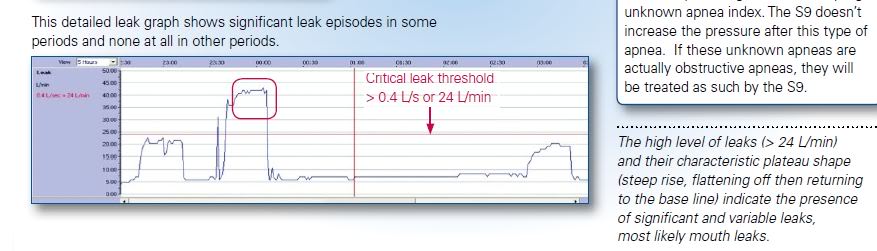
The pattern easy enough to identify. Do we know with absolute certainty that this kind of a pattern is most likely a mouth breathing leak? Of course not but we can often make an educated guess. Plateau type leaks combined with using a nasal mask interface and waking up with a dry mouth usually points to mouth leaks. Whether the mouth leaks are serious enough to warrant doing something about depends on their severity, both in terms of how large the leaks are and in how much they seem to disturb your sleep.
It's also important to point out again that two of the three probable periods of mouth breathing in that last example stay below the ResMed Redline: In terms of the efficacy of the CPAP therapy, the two smaller mouth breathing leaks are not serious enough to worry about. This runs counter to the commonly accepted notion that you loose all your therapy pressure any time you open your mouth while using a nasal mask: The amount of air you lose through an open mouth depends on a lot of factors, most notably the placement of the tongue. If the front 1/3 to 1/2 of your tongue is firmly planted on the roof of your mouth behind your top front incisors, the tongue effectively blocks off the oral cavity from the upper airway. And if you happen to open your mouth with your tongue in that spot, any mouth leaking may be very minimal as long as you are continuing to breath through your nose. If you start breathing through your mouth, however, the tongue will slip from that position, and as the tongue moves down away from the roof of the mouth, more air will be able to leak out of the open mouth.
Many people do switch to full face masks because of suspected or known mouth breathing issues. In a full face mask, you can open and breathe through your mouth without losing pressure. (Mouth breathing inside a FFM may still lead to serious dry mouth issues, however). But many people using FFM still have leak lines that have long plateau patterns reminiscent of mouth breathing. And it is not uncommon for these long plateau leaks to be large enough to be scored as Official Large Leaks. Since mouth breathing is not the (direct) cause of such a leak when you are using a FFM, what is? The most likely cause is the relaxation of the facial and jaw muscles after the mouth has opened. As we sleep, these muscles relax and the facial tissue around the mouth and chin starts to sag. If the lower face sags or relaxes enough, the mask may pull away from the chin and create a potentially large leak. It's also important to remember than FFM have a much larger footprint on the face, and hence there is more surface contact between the mask and the face, and that also can make it harder to seal a FFM in the first place.
Annoying Leaks
There are three types of leaks:
- Leaks that are both long enough and large enough to adversely affect your CPAP therapy;
- Leaks that are not long enough or large enough to adversely affect your CPAP therapy, but which are annoying enough to disturb the overall quality of your sleep; and
- Leaks that are not long enough or large enough to adversely affect your CPAP therapy and which do not disturb your sleep.
You only need to work on fixing the first two types of leaks. Small leaks which do not wake you up or lead to obvious restlessness can be ignored. Indeed, the efforts to try to eliminate the last of these small leaks may actually create problems in terms of overall comfort and your ability to get to sleep and stay asleep.
Long, large leaks need to be addressed because they affect your therapy, and ineffective CPAP therapy night after night will not allow you to feel at your best. If your leaks are frequently in Official Large Leak territory, you need to spend the time needed to figure out what's causing the leaks. Make sure your mask is the correct size and make sure you know how to correctly fit it at the beginning of the night: Overtightened headgear can cause serious leaks as can masks that are too large or too small for your face. If the large leaks seem to be caused by significant mouth breathing or facial relaxation and you are using a nasal mask or a nasal pillows mask, you may need to consider a chinstrap, or taping your mouth, or switching to a full face mask. If you're already using a FFM and the problem is facial relaxation, a mask liner or a chinstrap may help. Or you may need to add a special "anti-leak strap" for FFMs. ("Pad A Cheek" sells them.)
But small leaks that irritate you or wake you up or keep you from getting (back) to sleep prevent you from getting a genuinely good night's sleep. So any leak that disturbs sleep is unwanted-- even if it is tiny.
So an important question that a lot of CPAP users face is: How much should I do to try to eliminate all my leaks?
And the answer is, "It depends."
If your leaks stay below the Official Large Leak line for your machine and you seem to be sleeping soundly through them and your mouth is not too dry in the morning, you may very well decide to not do anything at all.
Some people aren't so lucky: It's clear that their leaks are either too large or too long or simply too annoying for them to get high quality sleep: If you are already super-sensitive to every little thing then you may need to take some extra measures to limit your leaks (both big and small). You have to be able to sleep first and fragmented sleep for any reason will totally mess up sleep architecture and the normal sleep cycles and the time spent in each sleep stage. If you wake up 20 times a night fiddling with leaks (whatever the cause) you are going to feel pretty bad the next day. Heck, if you wake up 20 times a night for any reason (even reasons you can't point a finger at) you are going to feel it the next day because if you remember a truckload of awakening, it's likely that you also had a fair number of awakenings that you don't remember also. And fragmented sleep in general just kills the body's ability to make use of the normal restorative powers of sleep.
And some people find themselves in the middle: Leaks sometimes seem to cause problems. Or perhaps certain types of leaks cause problems, but they can sleep through other types of leaks. If you find yourself in this situation, use some common sense when evaluating your leaks. How big of a problem is it really? And is the cure more of a problem than the leak? Dry mouth may or may not mean that you are seriously impacting your therapy with mouth breathing. And if your mouth leaks seldom reach Official Large Leak territory, you have to weigh the potential discomfort of wearing a chinstrap, taping your mouth, or using a FFM against the potential problems caused by the non-Official Large Leak mouth leaks. This is a personal call and has to be made on an individual level. Some people will be more comfortable having less leaks and more stuff on their face; others will be more comfortable sleeping with a few more leaks and (a lot) less stuff on their face. As long as your leaks are not staying in Official Large Leak territory for excessive periods of time night after night, the best decision is the one that gives allows you to sleep most soundly with the fewest wakes.
Why are Large Leaks an Issue?
We've looked at how each manufacturer defines an Official Large Leak, we examined leak lines in order to figure out how to tell if leaks are a significant issue, and we've looked at some causes for leaks. But we haven't actually looked at why Large Leaks cause problems for our CPAP machines and how those problems may affect our therapy.
When we use a CPAP, our upper airway is part of a "semi-closed pressurized system" comprising the blower, the tube, the mask, and our upper airway. The system is "semi-closed" because there is an intentional leak: The system is designed to intentionally lose air through the exhaust vents. The desired pressure is maintained in the system by constantly supplying enough new air into the system to balance out the amount of air being lost through the leaks: Our CPAP must blow enough air into the "semi-closed pressurized system" to replace the air lost through the exhaust vents in the mask.
It may help to draw an analogy: We can think about the CPAP machine, hose, mask, and our upper airway as a leaky inner-tube with a tire pump attached to it. We can keep the inner-tube fully pressurized and inflated as long as we keep adding air to the tube by pumping as much air into the tube as is being lost through the leak. But if we start losing more air through the leaks than we can pump in with the tire pump, the inner-tube loses pressure and starts to collapse.
It's the same idea with our CPAP machines: As long as the excess leak rate is not too high, the CPAP machine has no real trouble blowing enough new air into the system to compensate for the total leak rate. In other words, the CPAP can compensate for additional, moderate unexpected excess leaks by simply blowing more air into the system in order to maintain the same amount of pressurization. But there are limits to how much air can be lost before the machine simply can't keep up with its job: Once the total leak rate crosses into official Large Leak territory, the CPAP will have trouble adding enough air to the system to balance out the air leaking out of the system. And hence the machine will have trouble maintaining the desired pressure level.
And that's the fundamental problem with Large Leaks: If they last for a long enough time, the machine may become unable to maintain a therapeutic pressure inside the upper airway. And if the CPAP cannot maintain the necessary therapeutic pressure level, the upper airway becomes more vulnerable to collapsing. Which means that the CPAP machine is less effective in preventing apneas and hypopneas from occurring, and so the CPAP therapy itself is compromised.
But there is another problem a full efficacy CPAP machine faces when the leak rate approaches or stays in official Large Leak territory for any length of time: The breathing itself becomes more difficult to track. CPAP machines track our breathing by measuring subtle changes in the back pressure, but when the leaks start to approach the boundary of Large Leak territory, the "signal noise" caused by the leaks makes it harder for the machine to distinguish the subtle changes in back pressure that are used to detect the breathing. This can cause the Flow Rate data to become distorted and garbled; often times the perceived amplitudes of the inhalations and exhalations are significantly reduced even though normal breathing may be occurring. The following figure is from the discussion in the Clinical Overview for the DeVilbiss IntelliPAP AutoAdjust concerning what happens in the presence of excessively large leaks:
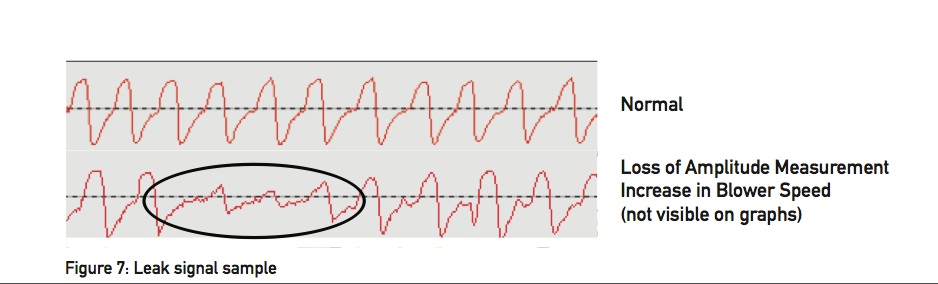
This inability to properly trace the breathing, of course, means that it becomes difficult or impossible to detect and properly score apneas and hypopneas should they occur during a prolonged period of Large Leaks.
Here's a close up of the large leak in SleepyHead 0.9.3:
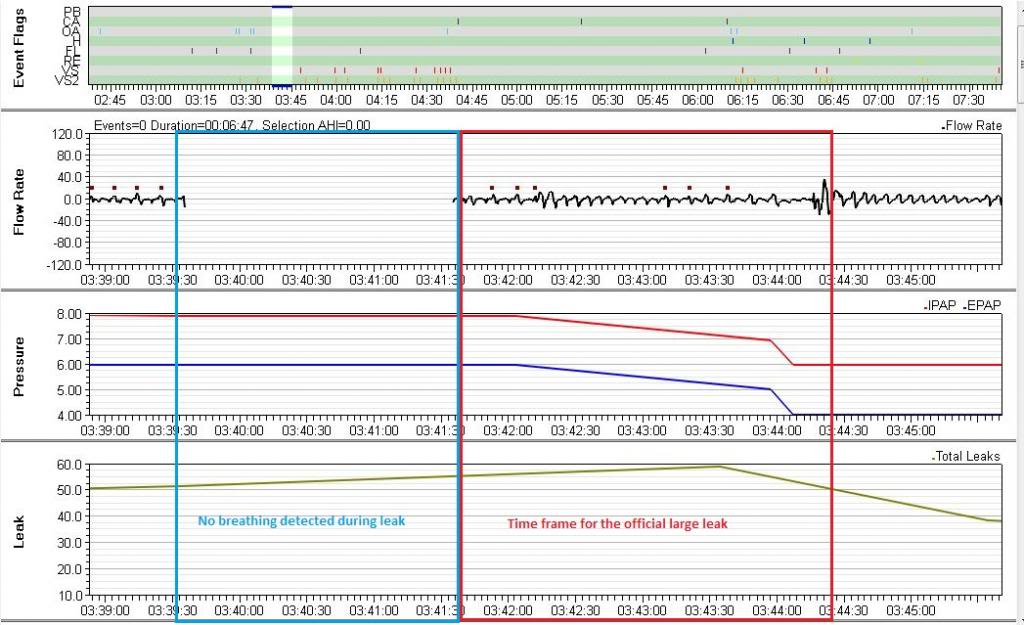
In SleepyHead, we see a break in the wave form preceding the biggest bump on the Leak graph. In Encore, that break in the wave form was flagged as a "breathing not detected period". The official Large Leak was scored as soon as the patient's BiPAP found a trace of her breathing pattern.
SleepyHead reports that the maximum leak rate topped out at 57.96 L/min, which is 2.5 to 3 times her usual, expected leak rate of 20-25 L/min; the official Large Leak starts when Total Leak graph crosses the 55 L/min line.
Notice how the wave form is severely compressed near the 0 line just before and just after the gap in the wave flow. This indicates that the patient's BiPAP could not reliably determine whether there was much air going into or out of the patient's lungs. And when the wave form picks up after the gap, it's still pathetic looking. It has none of the characteristics of what her wave form is usually like when she's awake enough to turn her BiPAP off and back on. So she's fully asleep during this leak.
And notice all those Pressure Pulses (the little boxes) right before the gap in the wave form and right after the wave form pics back up? It's likely those PPs are being used by the BiPAP to try to figure out if there's a live, breathing person at the other end of the hose. Perhaps the BiPAP "realizes" that these periods of very low variation in the wave flow are way too long to be a typical apnea or hypopnea, and that's why they are not flagged as such. But it also gets so befuddled about what it's seeing in the wave form data, that the BiPAP concludes she must not be breathing through the mask and so it quits recording Flow Rate data form during the time it cannot determine any meaningful breathing pattern. When this patient showed her DME this wave form pattern (in a different context), the Respiratory Therapist referred to it as a "patient disconnect". (And yes, that tern is bothersome because "patient disconnect" seems to imply that the patient disconnected the machine from her nose, when she did not do that here or anywhere else). But for now on, we'll call those wave patterns "patient disconnects" even though we don't like that language at all.
A couple of minutes after the BiPAP detects the "patient disconnect", it finds rudimentary evidence of breathing again, so it starts recording the Flow Rate data. But by this point the leak rate has also grown to about 55 L/min and the BiPAP decides to flag this as an official Large Leak. As in-- there's breathing present and the leak is now large enough to meet that unknown Philips Respironics standard of Large Leak. And it's important to note that almost as soon as the Large Leak is detected, the patient's BiPAP starts to lower the pressures: First from 8/6 to 7/5 and then more sharply from 7/5 to 6/4. Her BiPAP is attempting to help limit or even fix that Large Leak by lowering the pressures---exactly as the description of the Philips Respironics Auto algorithm says it is supposed to do in the presence of Large Leaks.
As far as accuracy of recording events during this Large Leak: Because her BiPAP can barely detect a breathing pattern, it's clear that the usual definitions used to flag OAs, CAs, and Hs are going to be difficult to apply: They all rely on a reasonably accurate baseline of the current airflow into/out of the lungs and that baseline is calculated using several minutes worth of data. Because the breathing pattern is barely there, it's almost impossible for the machine to detect enough of a decrease in airflow to trigger flagging an OA or a CA or an H throughout the Large Leak (and even in the part of the longer, not-quite-so-large leaks immediately preceding and following the official Large Leak itself.) And hence there's no good reason to believe that this time frame is really as "event-free" as the event chart makes it appear to be: After all, you can't detect an apnea or hypopnea if you can't detect the breathing pattern in the first place.
Beyond AHI: Apneas and hypopneas in the Flow Rate graph
Most sleep doctors and most OSA patients never really concern themselves with detailed efficacy data beyond the nightly and long term AHI data. And that's ok: If the nightly AHIs are almost always below 5.0 and you're feeling well, there's really no need to look at the detailed data available in SleepyHead about each and every event the machine recorded over night. But if you're a data hound, the stuff you can see in the Flow Rate data can be fascinating. And if you're not feeling as well as you hoped with CPAP therapy, sometimes examining the Flow Rate data in more detail can shed some insight into what might be going on.
The information on this page is written for the curious CPAP users who simply wants to know more about what the Flow Rate data shows and what it may indicate about the quality of therapy. None of this information should be considered medical advice. If you are experiencing problems with your CPAP therapy, you should consult your sleep doctor.
Flow Rate graph: A trace of every breath you took
When we use a CPAP, our upper airway is part of a "semi-closed pressurized system" comprising the blower, the tube, the mask, and our upper airway. The system is "semi-closed" because of the intentional leakage built into the mask to prevent re-breathing. A full efficacy data CPAP measures the back pressure at blower end of "system" and uses that data to calculate the air flowing into and out of our lungs all night long. The resulting data is called the Flow Rate data, and the Flow Rate graph provides a trace of very breath you took all night long.
To understand how to read a Flow Rate graph, it helps to zoom in to the point where the individual breaths can be seen:
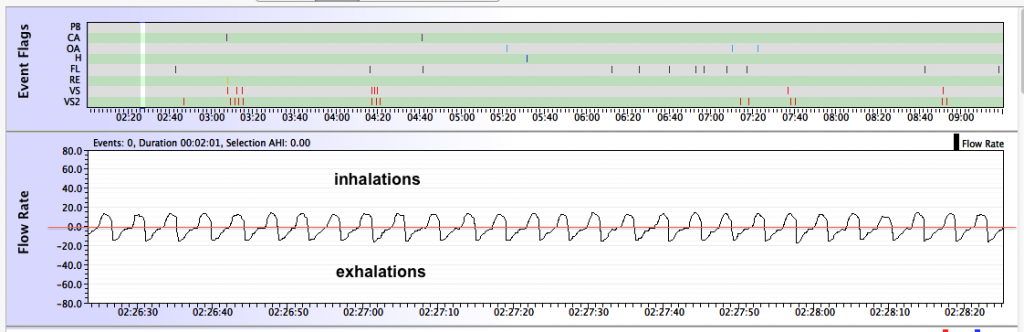
The y-values are measured in Liters per minute (L/min). When the Flow Rate is positive (above the horizontal line labeled as 0.0), the air flow is going into the lungs and you are inhaling. When the Flow Rate is negative (below the horizontal line labelled as 0.0), the air flow is going out of the lungs and you are exhaling. The farther away from the 0.0 line, the more rapidly the air is moving. So a large positive bump represents a strong, deep inhalation, whereas a large negative bump represents a strong, deep exhalation. The transition between inhalations and exhalations occurs when the Flow Rate graph crosses the 0.0 line. Pauses in breathing show up as flat spots in the Flow Rate at the 0.0 line.
Normal sleep breathing, such as shown in the above graph, is very regular in the size and shape of the inhalations and exhalations. Normal sleep breathing is usually much more regular than normal wake breathing, and typically the size of the inhalations and exhalations is smaller in sleep breathing than in wake breathing.
Basic scoring criteria for apneas and hypopneas
Each event that is scored by your machine shows up as a tick mark in the Flow Rate graph. Zooming in on the Flow Rate curve often shows exactly why the event was scored; but sometimes it is not clear why an event was (or was not) scored. And since our CPAPs do not have EEG data, they cannot tell when we are awake and when we are asleep. Hence your CPAP will score "events" that meet the definitions in their scoring algorithm even if you are wide awake.
Each machine's manufacturer has its own algorithms for scoring (and classifying) apneas and hypopneas. These algorithms are not perfect-- we'll look at that later. But they are very good.
Rather than looking at each individual CPAP maker's definitions of apnea and hypopnea, we'll generalize the basic concepts that underlay all their algorithms
- Moving Baseline Flow Rate. All full efficacy CPAPs compute a moving baseline flow rate using several minutes worth of data. The typical time frame is a five minute window of some type: The machine looks at all the breaths in the last five minutes and uses that information to compute an average or baseline flow rate. (The particulars of how this baseline is computed are NOT the same on all CPAPs, but those particulars don't change a basic understanding of how events are scored.) It's enough for now to think of the moving baseline flow rate as the "average" size of your inhalations for the last five minutes or so. Apneas and hypopneas are scored when there is a measurable and significant decrease in the Flow Rate as compared to the moving base line average and that decrease lasts for at least 10 seconds.
- Apneas. Typically an apnea is scored when the Flow Rate is reduced by at least 90% from the moving baseline average for at least 10 seconds. In other words, during a machine scored apnea, the air flow into (and out of) the lungs is less than 10% of the moving baseline airflow. This is enough of a reduction in airflow that the Flow Rate curve typically looks pretty flat and it's clear that little or no air is moving into or out of the lungs.
- Hypopneas. Typically an apnea is scored when the Flow Rate is reduced by at least 50% from the moving baseline average for at least 10 seconds. In other words, during a machine scored hypopnea, the air flow into (and out of) the lungs is less than 50% of the moving baseline airflow. The actual amount of air flow reduction needed to score a hypopnea depends on the manufacturer. DeVilbiss allows the criteria for scoring a hypopnea to be customized: The reduction in airflow can be set anywhere between 30% and 70%.
It's important to remember that on an in-lab sleep test (PSG), you have to be asleep at the beginning of the event for it to be scored as a sleep disordered breathing event. And that means that EEG data must be used in scoring real sleep disordered events on a PSG. But our CPAPs do not have any EEG data to work with, and any time the Flow Rate meets the manufacturer's definition of an apnea or hypopnea, the machine will score the event. The working assumption is: If you have the mask on your nose, there's a high probability that you are asleep and the event is "real." Whether the assumption that you are most likely asleep, however, may not be a valid assumption in some circumstances. We'll return to this idea in a bit.
Obstructive and central apneas
On an in-lab sleep test (PSG), each apnea will be classified as either an obstructive apnea or central apnea. The data from the belts around the chest and abdomen are used to distinguish between the two types of apnea on a PSG. If the belts indicate that the patient is trying to breathe, but no air is getting into the lungs, then it's assumed that the problem is that the upper airway has collapsed and the apnea is scored as an obstructive apnea. But if the belts indicate that the patient is making no effort to breathe, then it's assumed that the problem is that the brain has "forgotten" to send the signal to the diaphragm and lungs to inhale. The patency of the airway is irrelevant when scoring a central apnea on a PSG because the main problem is with the brain's forgetting to tell the diaphragm and lungs to breath. And it's possible for the airway to collapse during a central apnea.
But our CPAPs have no way to determine the effort to breathe. Hence CPAPs cannot distinguish between obstructive and central apneas in the same way that the technician monitoring a PSG does. Originally full efficacy data CPAPs did not try to distinguish between obstructive and central apneas. (The Fisher & Paykel Icon still does not try to distinguish types of apneas.) But when manufacturers started designing Auto CPAPs, a potential problem had to be addressed in the Auto algorithms: A minority of CPAP users are sensitive enough to pressure to develop problems with pressure-induced central apneas. And the tendency to have problems with pressure-induced centrals is more pronounced the higher the pressure setting on the CPAP. Hence early APAP Auto algorithms often were designed to NOT increase the pressure in response to apneas scored at pressures of 10cm or greater. In an effort to get around this difficulty, many of the current generation of full efficacy CPAPs make an effort to distinguish between apneas are presumed to be obstructive and those that are presumed to have a high probability of being central, and an APAP with such a "central apnea detection" algorithm can be programmed to respond to the apneas classified as obstructive and ignore the other apneas.
ResMed and Philips Respironics CPAP machines use (different) proprietary algorithms to test the patency of the airway and use the result to classify each apnea as a clear airway apnea (CA) or an obstructive apnea (OA). When the data from the algorithm leads to an ambiguous result, the apnea may be scored as an unknown apnea (A or UA). Both ResMed and Philips Respironics Auto machines will increase the pressure in response to clusters of OAs, but they will not increase the pressure in response to apneas scored as CAs.
DeVilbiss machines use a very different algorithm to classify each apnea as an apnea (A) or a non-responding apnea (M or NRA). A DeVilbiss Auto machine will increase the pressure in response to events classified as "apneas", but it will not increase the pressure in response to "non-responding" apneas.
As near as I can tell, Fisher & Paykel machines do not try to distinguish the type of apnea. And I have not been able to find any specific information about how the Fisher & Paykel Icon responds to machine scored apneas.
It's also important to remember that the ResMed and Philips Respironics algorithm for distinguishing between OAs and CAs and DeVilbiss algorithm for distinguishing between As and NRAs are not infallible. They are prone to misclassifying apneas under certain circumstances. For most users, it's not a huge problem, but for a small number of users, it can be an issue. We're not familiar enough with the DeVilbiss alogrithm to have a good sense of its limitations. But both the ResMed and Philips Respironics algorithms are based on using variations in the CPAP pressure to test the patency of the upper airway. As such they both have the same broad characteristics:
- A CA scored by either the ResMed or Philips Respironics CA algorithm is very likely to be a "real" CA in the sense that the airway is clear (open). As such, a real OA is not very likely to be mis-scored as a CA on either a ResMed or Philips Respironics machine.
- Scoring a real central apnea (as scored on an PSG) does not depend on the patency of the upper airway; hence there is a higher probability that a real CA may be mis-scored as an OA by the Philips Respironics and ResMed CA detection algorithms
- Both the Philips Respironics and ResMed CA-detection algorithms are more likely to have problems detecting CAs at higher pressures. In other words, as the pressure increases, the chances that a CA is mis-scored as an OA increase
Other flagged events
In addition to scoring apneas and hypopneas, many CPAP machines score snoring and/or flow limitations (FL). The way machines score this things varies quite a bit, and they are discussed at length in 10. Snoring Data and 11. Flow Limitations.
In addition to scoring OAs, CAs, Hs, snoring, and FLs, the Philips Respironics System One machines also score respiratory effort related arousals (RERAs) and periodic breathing (PB) in the events table with flags on the Flow Rate curve.
RERAs
On an overnight PSG, a RERA is scored when there is evidence of increasing respiratory effort that ends with an EEG arousal. Not all labs score RERAs, by the way. The line between RERA and an AASM Rule 4B "hypopnea with arousal" is a bit arbitrary: RERAs don't have have last 10 seconds, but 4B hypopneas do; RERAs do not require a 50% reduction in airflow, but 4B hypopneas do. And a RERA requires an EEG arousal, whereas a Rule 4B hypopnea requires either an arousal OR an O2 desat of 3%. Finally a RERA may nor may not have an O2 desat. When a lab chooses to score RERAs, the lab will usually compute both an AHI and an RDI:
- AHI = (number of OAs + CAs + Hs scored)/(total sleep time)
- RDI = (number of OAs + CAs + Hs + RERAs scored)/total sleep time)
There are people whose PSG indicates that they a normal diagnostic AHI (less than 5), but who experience enough RERAs for the RDI to be seriously elevated. Such people often wind up with a diagnosis of upper airway resistance syndrom (UARS) instead of OAS. The connections and differences between UARS and OAS are still being debated in the sleep medicine community. But the usual treatment for UARS is CPAP therapy since CPAP can be used to smooth out the breathing and prevent the RERAs from happening.
Since a RERA requires an EEG arousal to be scored and there is NOT a clear definition of how much the flow rate must be reduced for a RERA to be scored, most CPAP machines do not attempt to flag RERAs. But Philips Respironics has developed a proprietary algorithm for scoring what it believes are RERAs. Since there is no EEG data, the Philips Respironics RERA algorithm is based on a statistical analysis of what the wave flow for real RERAs on PSGs looks like: Loosely, the Philips Respironics RERA algorithm looks for evidence of increasing respiratory effort (i.e. "flow limited breathing") followed by one or more "recovery" breaths. When we look at the RERAs scored in our sample patient's data, it's sometimes difficult or impossible to see both the "evidence for increasing respiratory effort" and the "recovery breaths". We've also noticed that the placement of the RERA tick mark is far less consistent: Sometimes it appears at the beginning of the RERA, sometimes it appears at the end, and sometimes it appears in the middle. But every now and then we see a RERA where it is easy to see why it was scored:

Because the RERA algorithm is proprietary and is based on just flow rate data rather than (flow rate + belts + EEG), it's important to understand that RERA flagging by the Philips Respironics machines should be considered an "extra" that is probably not always accurate. The RERA algorithm probably flags things that aren't real RERAs and it probably misses some real RERAs as well.
Nonetheless, if your sleep study showed a large number of RERAs the Philips Respironics RERA scoring algorithm may be useful for partially monitoring how well the CPAP is doing in terms of preventing RERAs from occurring.
Periodic Breathing
Philips Respironics machines flag breathing that meets their definition of periodic breathing (PB). On the Philips Respironics web pages PB is defined as, "Periodic breathing is defined as alternating periods of hyperventilation with waxing/waning tidal volume..." Typically the waxing and waning pattern must be quite regular in visual appearance and it must present for at least a minute or two for PB to be scored. PB is flagged with a green back ground on the flow rate data. Often, but not always, there will be CAs (or Hs or sometimes OAs) scored at the nadir of the cycle. Sometimes the System One will only flag the most obvious part of the cycle:
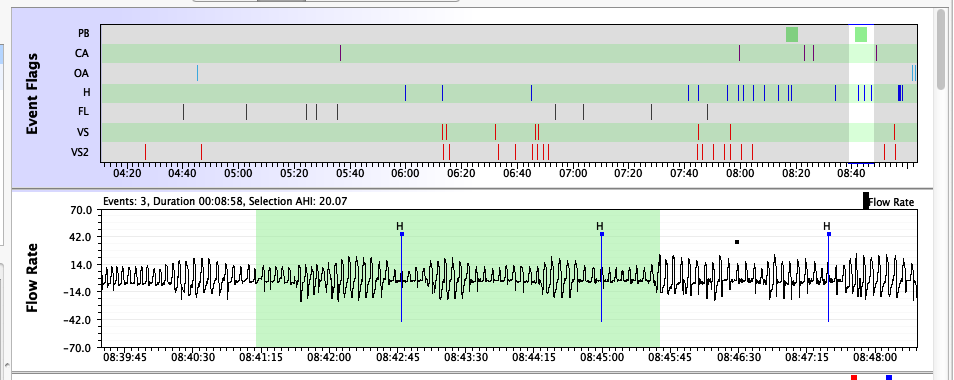
A bit of PB now and then is nothing to worry about. However, there is one form of PB that is called Cheyne-Stokes Respiration (CSR) that is clearly associated with some forms of heart disease, including congestive heart failure. CSR is very regular and has a CA at the nadir of the cycle (although the CA may be mis-scored as an OA). If you have serious heart disease and you see a lot of PB scored in your flow rate data, it is worth mentioning it to your cardiologist as well as your sleep doctor.
Detecting Periodic Breathing on other CPAPs
Once you know what PB looks like, you can often spot suspicious patterns by simply scrolling through the Flow Rate data in with a 5-10 minute window. Any periodic waxing/waning patterns will be show up at that magnitude. Whether this is worth doing on a regular basis is another question altogether. Unless you have a co-morbid condition that is associated with PB (such as congestive heart failure), PB is not something you need to spend much time worrying about or trying to locate in your data.
Here's an example of PB that may be CSR pulled from a ResMed machine:

Wake breathing and "False" events (Sleep-Wake-Junk)
Because the scoring of an apnea or a hypopnea depends on the moving baseline airflow, the actual airflow recorded during an apnea or a hypopnea can vary. This becomes important during periods when you are not soundly asleep. Wake breathing is controlled by the voluntary nervous system and it is much more variable than sleep breathing. Because of this variability it is not uncommon for OAs, CAs, and Hs to be scored during periods when you are awake: A few minutes of conscious deep yoga style breaths followed by a return to normal wake respiration may meet the criteria to be scored as an H. When we're tossing and turning in bed, it's not uncommon to hold our breath for a few seconds while concentrating on turning over or fixing the bed pillows and covers; if the pause in our breathing is close to 10 seconds, it can be mis-scored as a hypopnea. And some people's wake breathing patterns are more susceptible to being misinterpreted as sleep disordered breathing than others. These sleep/wake/junk dozing periods are most likely to happen at the beginning or end of the night, particularly if you are in the habit of lying in bed without being sound asleep.
Sometimes patients will lie in bed trying to get back to sleep if they're not quite ready to get up; sometimes they can be restless before admitting that they're not likely to get back to sleep. If you're like this and look at your data after one of these mornings, you may see a lot of sleep/wake/junk breathing. Here's a close up of what sometimes happened when our sample patient lied in bed unsuccessfully trying to get back to sleep:
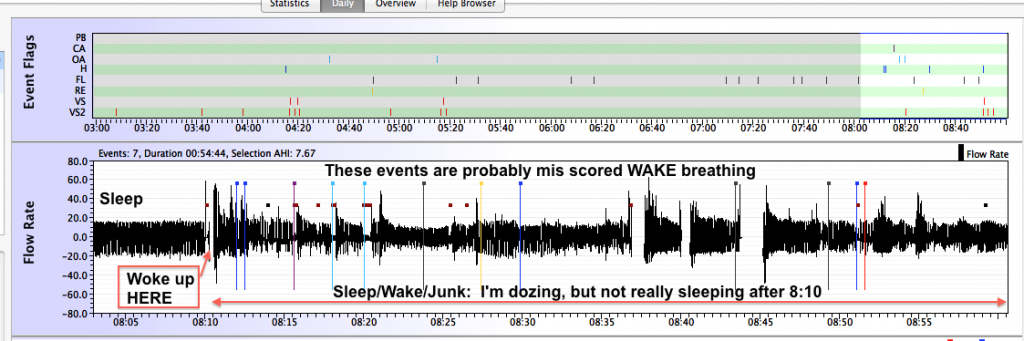
In this data, it's clear that the patient never got soundly back to sleep not only because of the large number of (false) events, but also because she turned the BiPAP off and back on three additional times after the first wake around 8:10 before finally deciding to crawl out of bed at 9:00. During this wakeful period, 4 Hs, 1 CA, 2 OAs, 3 FLs, 1 RERA, and some snoring were all scored. All of them are likely artifacts of her wake breathing and/or irregularities in her breathing scored as she was just starting to doze before waking back up. On a PSG, most or all of these events would probably not be scored based on EEG data-- an event has to start in SLEEP in order to be scored as sleep disordered breathing.
Distinguishing this kind of sleep/wake/junk (SWJ) breathing from periods of seriously sleep disturbed breathing periods that indicate your CPAP therapy may not be optimized is not particularly easy. But extremely restless looking periods at the beginning or end of the night are more likely to be SWJ. And if you know you were awake for long periods of time during the night, clusters of events during the times you were awake (or restless) are likely to be SWJ.
Sleep transition breathing and "False" events
Sleep transition breathing also poses problems for our machines. The control of respiration has to be handed off from the voluntary nervous system to the autonomous nervous system. it is not uncommon that during the transition process, the airflow into the lungs drops (and a breath or two is skipped) as the body resets the CO2 trigger for inhalation. On a PSG, these "sleep transitional central apneas" are not scored because they are not part of sleep disordered breathing. But our machines cannot tell that we're in the process of transitioning to sleep, and it's not uncommon for "false" events to be scored just as we're drifting off to sleep.
Here is an example of a sleep transition central apnea from our sample patient's data:
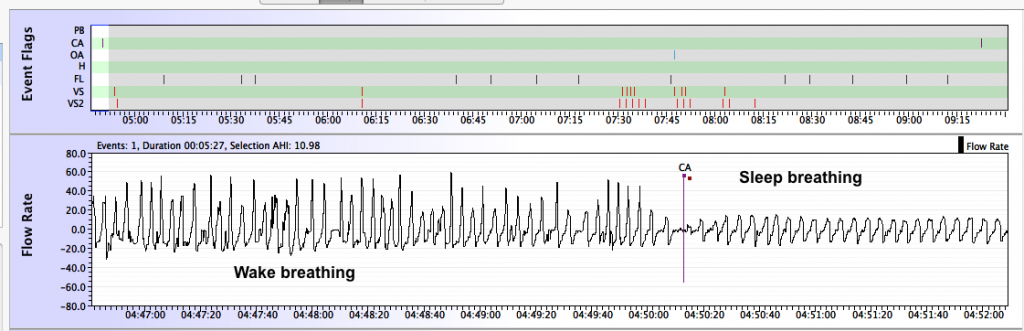
Contrast the above sleep transitional central apnea with what appears to be a real central apnea:
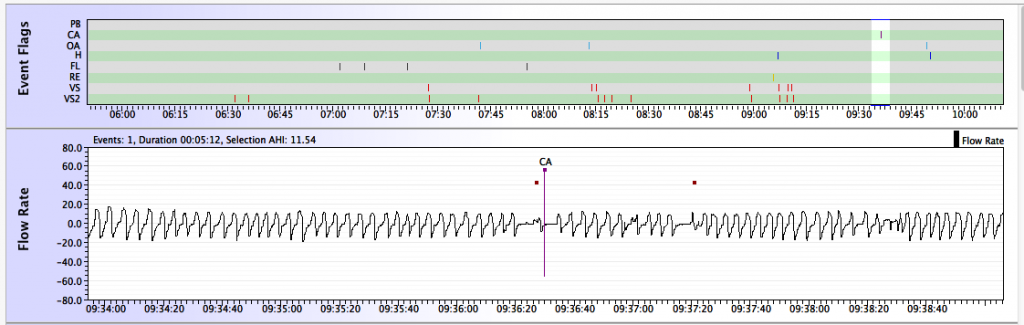
Lengths of individual events
SleepyHead has a neat tool that both lets you zoom in on a particular event and (estimate) how long it lasted. Between the Calendar and the AHI table in the standard view of the Daily Data table there is a navigation menu that looks like this:
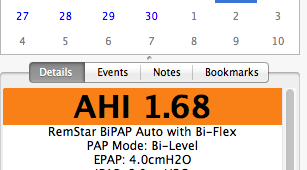
Clicking on the Events tab changes the look of the Left Side Bar; once Events is selected, the Left Side bar looks like this:
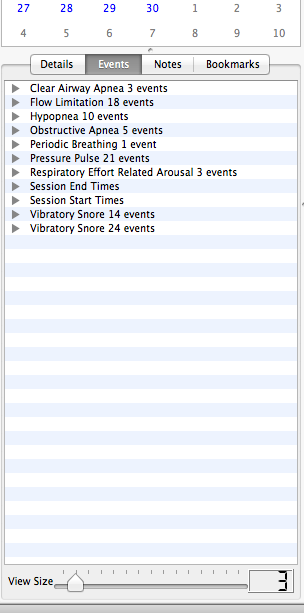
You will notice this is a list of the kinds of events that were recorded for the night. Clicking on the little triangles by each event type brings up a list of the the individual events of that type:
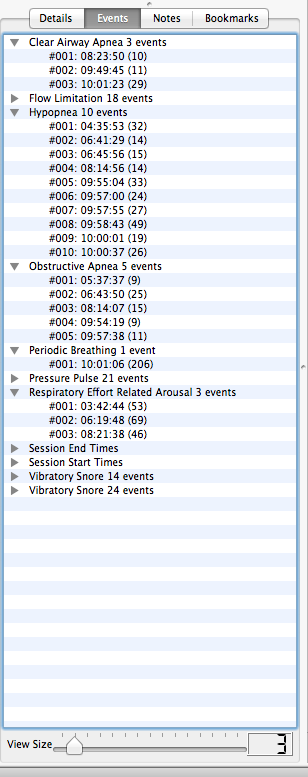
For CAs, Hs, and OAs on an S9, the number in parenthesis beside the event is the length of the event measured in seconds. On other machines, those numbers are event markers of some sort and they may or may not provide a reasonable estimate of the length of time (in seconds) of the event.
- ResMed S9: The numbers in parenthesis are the length of the event measured in seconds.
- Philips Respironics System One: The numbers are event markers. For CAs, OAs, Hs, PBs, and LLs, the numbers are usually a good approximation of the event length measured in seconds. For RERAs, it appears that the number is a good approximation of the event measured in seconds. For VS, VS2, and FL it is not at all clear what the meaning of the numbers is. SleepyHead uses the VS2 numbers to draw the Snore graph; presumably the higher the number attached to a VS2, the louder OR longer the snoring. It's not clear which. For more information on how the Philips Respironics scores snoring see 10. Snoring Data.
- DeVilbiss IntelliPAP: The numbers in the parenthesis are usually single digit numbers and it is not clear what their meaning is. Since the IntelliPAP does not record Flow Rate data, it is impossible to see whether there is some connection between these numbers and the lengths of the events.
- Fisher & Paykel Icon: The numbers in parenthesis seem to always be 1, and hence they are not related to the length of the event. You can zoom in on each event in the Flow Rate curve and estimate the length of the event visually.
Clicking on a particular event in the Events list immediately zooms all the Daily graphs into a close up view of the chosen event. The time frame for the event is controlled by the number on the slider bar at the end of the Events list: The smaller the number, the closer we zoom in:
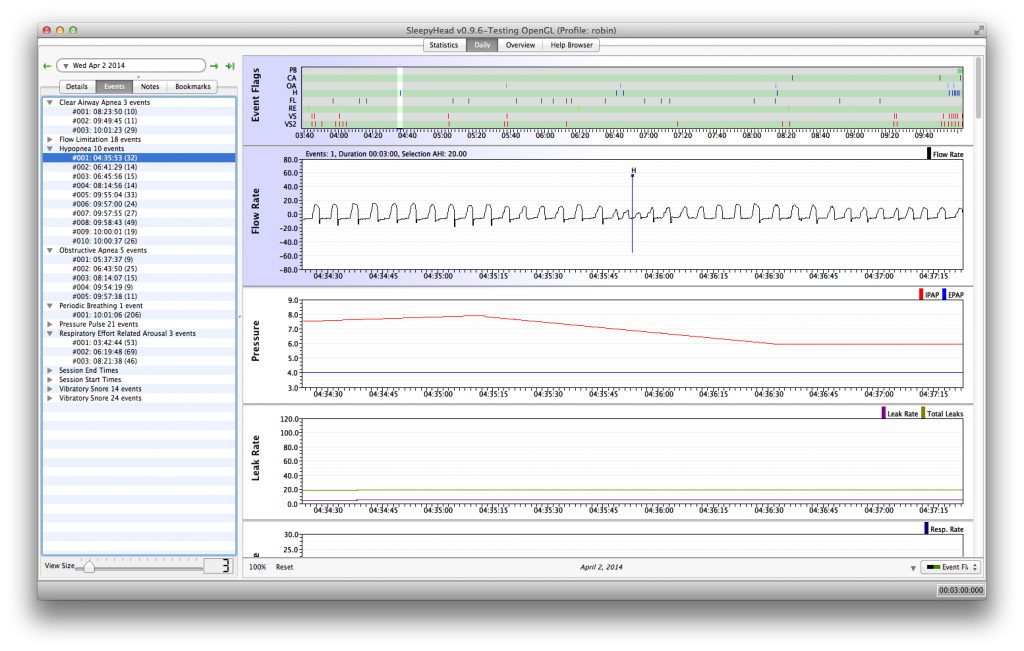
This particular hypopnea's flag is more or less in the middle of the hypopnea. Most of the time the flag is closer to the end of the event, but there is some variability. Another thing that's worth pointing out is that the patient's BiPAP is in the middle of decreasing the IPAP as part of the Philips Respironics "search" algorithm; the isolated H does not cause the machine to increase the IPAP and that's a bit counter intuitive to some CPAP users. But it is how the Philips Respironics Auto algorithm works: It ignores isolated Hs and OAs; pressure is increased for events only if two or more events occur very close to each other.
Clusters of events
One common concern CPAP users have about their data are clusters of events. It's important to understand that your CPAP machine is not going to prevent every apnea. If you have a bad night now and then with some clusters of events, it's not something to worry too much about. But if you tend to see dense clusters of events on most nights, your CPAP therapy may not be optimized.
Figuring out what's causing clusters of events can be difficult: Sometimes clusters of events occur in REM sleep. Sometimes clusters appear during back sleeping. Sometimes clusters of events are just sleep/wake/junk breathing. Occasionally clusters of events may be an indication that you're in the unlucky 10-15% of CPAP users who have problems with pressure-induced central apneas.
There's no clear way to tell what caused any particular cluster of events. Our CPAPs do not have EEGs and there's no way to definitively tell when REM sleep is occurring in the data. Likewise our CPAPs have no position detector, so the data can't directly tell us whether supine sleep is the problem. If you remember being awake or restless at certain period in the night, then it may be possible to identify a cluster as probably being sleep/wake/junk, but it's not uncommon to have no real memories of a restless period during the middle of the night. Long clusters of central apneas at times you think you were asleep obviously raise the question about pressure induced centrals.
If your diagnostic sleep study indicated that your OSA is much worse in REM and the clusters are roughly 90 minutes apart with longer clusters towards the end of the night, they may very well be REM related. If your diagnostic sleep study indicated that your OSA is much worse in supine sleep and you find yourself waking up on your back at times, then the clusters may be supine-sleep related. But there really is no way to tell for sure that clusters of events in your data are REM or supine sleep related. Sometimes its worth making the reasonable assumption that the clusters are REM or supine sleep related in these situations, and if the clusters are particularly persistent (as in they occur on most nights) and nasty (as in they involve a lot of events), it's worth checking with your sleep doctor since a (small) increase in pressure may help break up the clusters. But if the clusters continue after one or more pressure increases, more formal investigation into their cause may be needed.
How APAP machines respond to events
New CPAP users are sometimes surprised by the fact that their CPAP did nothing when an apnea was in progress. There's an assumption that the positive air pressure provided by the CPAP is supposed to "blast" through the obstruction and restart the breathing. But pressure is not used to try to "end" an on-going event. It's not even clear that 20cmH20, the maximum pressure delivered by a CPAP, would even be effective at trying to "blow" a collapsed airway open: 20cmH20 is not enough pressure to effectively blow up an ordinary balloon. In fact, 20 cmH20 is about the difference in atmospheric pressure between a very stormy, low pressure day, and a bright sunny high pressure day.
The basic idea in CPAP therapy is to provide (a small bit of) positive air pressure through the entire breath cycle to make it more difficult for your airway to collapse. This system is very good at preventing apneas and hypopneas from occurring, but it is not perfect: A few events will likely occur each night, but the overall number of events will be low enough to keep your treated AHI under 5.0, and probably well under 5.0, each night you use the machine. In other words, a well-adjusted CPAP makes it difficult, but not impossible for your airway to collapse.
CPAPs, of course, cannot respond to OAs and Hs by increasing pressure since they have one fixed pressure setting. APAPs do respond to OAs and Hs, but it's important to realize that an APAP will wait until the apnea or hypopnea is over before it increases the pressure. And even then, a typical APAP won't raise the pressure after each and every OA or H. Rather, APAPs will only raise the pressure in response to OAs and Hs if two or more events occur in a relatively small amount of time like 5 minutes or so. The rationale for this behavior is based on the AASM Clinical Guidelines for Manual Titration Sleep Studies. Isolated OAs and Hs are not necessarily indicative of a badly compromised airway: Even normal people have the occasional (frank) OA or H during their sleep. But two or more OAs or Hs occurring close together indicates that the current pressure may not be sufficient to prevent the airway from collapsing in the (very near) future. And since more pressure is needed to prevent future events from happening, the machine increases the pressure after the second (or latest) event in the cluster ends.
APAPs also respond to snoring and flow limitations by increasing the pressure. Snoring and flow limitations are considered precursor events to OAs and Hs. In other words, snoring and flow limitations are thought to indicate that the airway is compromised: It may be partially collapsed (but not far enough to score an H) or it may be just barely beginning to collapse. More pressure at this point will help hold the airway open and prevent further collapse, and hence, prevent OAs and Hs from occurring. It's worth noting that some brands of APAPs are very aggressive in how fast and how far they increase pressure in response to snoring or flow limitations.
So the overall goal in every manufacturer's Auto-algorithm is to increase the pressure just enough to prevent more events from happening in next few minutes and allow the breathing to stabilize. The idea is to avoid jacking up the pressure unnecessarily: That can lead to more unstable breathing, discomfort, and more pressure than is needed to keep the airway open most of the time. And once the machine is satisfied the breathing is indeed stable, the Auto-algorithm will decrease the pressure until there is evidence that the airway is once again in some danger of collapsing.
Each manufacturer's Auto-algorithm handles the details of how to handle the pressure increases and decreases in its own proprietary way. Some machines are more aggressive and increase pressure faster in response to snoring, flow limitations, and events. Some take small 1cm steps in increasing the pressure and then wait for a minute or more before increasing the pressure further. The Philips Respironics machines even have a search algorithm that periodically tests what happens to the Flow Rate curve when a modest pressure increase is applied even when there are no scoreable events (OAs, Hs, FLs, RERAs, and Snoring). And likewise, each manufacturer's algorithm has a different way of deciding when to start decreasing the pressure and how fast to decrease the pressure.
It's clear from reading informational material aimed at clinicians, that each manufacturer believes that they have the "best" algorithm. But what little information that has been published about independent bench trials seems to indicate that while real differences in the auto-algorithms can be quantified, the clinical significance of those differences is much harder to evaluate. This may be one reason that some sleep docs are so reluctant to prescribe APAP therapy as the first course of treatment for ordinary OSA.
Snoring Data
ResMed S9s, Philips Respironics System One CPAP and DeVilbiss IntelliPAP machines record snoring data. Fisher & Paykel Icons do not record snoring data.
How does a CPAP machine detect snoring?
CPAP machines do not have microphones attached to them. So your CPAP is not listening to the sound of your snoring. So how does it actually detect snoring? It analyzes the Flow Rate data.
When a person is snoring (at least when they're snoring loudly or persistently) there are some characteristic changes to the flow rate, and a full efficacy data CPAP's flow rate analysis algorithms can pick that up. Typical types of flow rate curves exhibiting sleep disordered breathing problems can look like any of the following images:
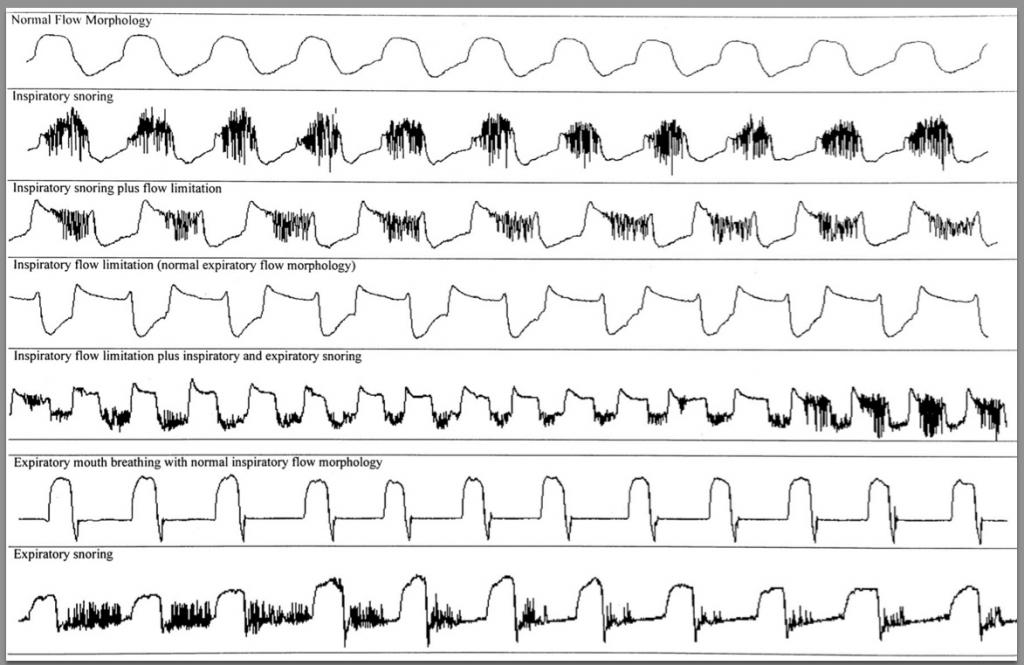
Snoring triggers oscillations in the flow rate curve. The larger and more persistent the oscillations, the worse (and louder) the snoring is. And that pattern of oscillations is what your CPAP uses to detect snoring.
Notice, too, that inspiratory snoring (snoring only on inhalations) has a different wave flow than expiratory snoring (snoring only on exhalations). It's also possible to snore on both the inhalations and the exhalations; in that case the oscillations appear on both the inhalation and exhalation parts of the flow rate curve.
Snoring data on a ResMed S9
Snoring data on a ResMed S9 is recorded as a function of time. At each time t, the machine assigns a "snore" number; SleepyHead graphs those "snore numbers." Here is the same Snore graph of the same 30 minutes of sleep displayed in both ResScan and SleepyHead.
The Snore graphs in ResScan and SleepyHead look pretty much the same, except for how the vertical axis is labelled. In ResScan there is a cryptic icon scale that implies that the higher the snore graph, the louder the snoring. Notice that if the snoring is really severe it may go off the top of the ResScan graph.
On SleepyHead, the y-axis is scaled from 0.0 to 5.0, with
- 0.0 corresponding to the "no snoring" icon on the ResScan graph
- 1.5 corresponding to the "medium/moderately loud snoring" icon on the ResScan graph
- 3.0 corresponding to "loud snoring" icon on the ResScan graph.
Typically anything that's over 3.0 on the SleepyHead graph has gone off the top of the scale in the ResScan graph.
While it is important to remember that the S9 has no direct way of determining the loudness of the snoring, it's also clear from the ResScan graph labels that snoring numbers above 3 represent more serious snoring than snoring numbers under 1. Somehow the S9 decides "how loud" the snoring is and assigns the snoring number based on both the amplitude and frequency of the oscillations in the flow rate curve.
Note: The S9 AutoSet and S9 VPAP Auto will react pretty aggressively to snoring. It is not uncommon to see substantial increases in pressure in response to snoring even if no OAs or Hs are being recorded.
Snoring data on a DeVilbiss IntelliPAP
Snoring on an IntelliPAP is recorded as a graph with respect to time in SleepyHead. But the graph is a "square wave" graph rather than a curve. Here's a picture of a typical IntelliPAP Snore graph from SleepyHead:
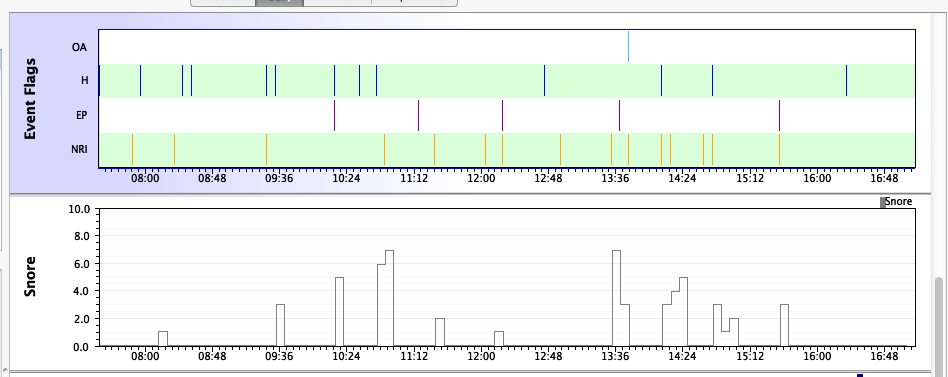
The meaning of the numbers on the vertical axis is unknown, but they are presumed to indicate loudness. I've seen IntelliPAP Snore graphs with Snore numbers as high as 30.
SleepyHead presents the snoring data very differently than the DeVilbiss software. In DeVilbiss's software package, the snore data is presented as "fat" tick marks on the DeVilbiss software's event table, which is shown below:
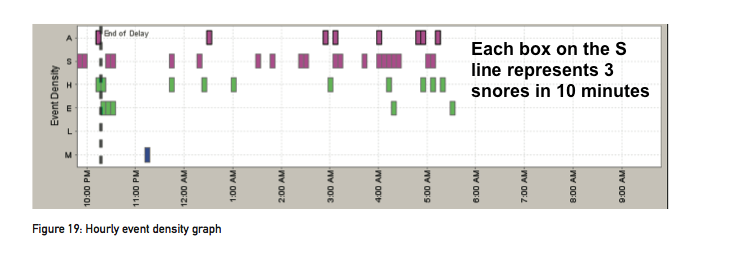
Each fat tick mark represents a ten minute time slot with at least 3 snores scored during that time period. Tick marks run together if there is snoring in consecutive 10 minute blocks.
Snoring data on a Philips Respironics System One
Please note the following: The way snores are recorded on the ResMed S9 machines is very different than the way it is recorded on the Philips Respironics System One machines. This information applies only to the snore data recorded by the Philips Respironics System One machines and how that data is reported in both the SleepyHead and Encore software packages.
All about Snoring Data on the Philips Respironics System One Machines
There's no official guide to how to interpret the Snoring information from the Philips Respironics System One as it is reported in either SleepyHead or Encore. In looking at Encore numbers, the assumption is that the higher the so-called "VSI" number is, the more serious the snoring is. But exactly how large that number needs to be before it's troublesome is not known. And for reporting snoring in SleepyHead, the snoring data was reverse-engineered from the Philips Respironics machines and the information on why Encore presents the snoring data the way it chooses to present it is pretty scarce...
And when you start analyzing the raw snoring data the decisions Encore makes on how to present the snoring data seems bizarre from a statistical point of view. (More on that later.)
After reverse-engineering the snoring data, it was discovered that the Philips Respironics machines were keeping track of two kinds of snoring data; there were two types of snore data Vibratory Snores (VS) and Vibratory Snores #2 (VS2). Those who had access to Encore Pro and had data from both straight pressure mode and auto mode were able to figure out just what the significance of those two kinds of snores are in the Encore/PR world are. Here's the run down as we now understand things:
VS snores
VS snores are recorded ONLY when a Philips Respironics machine is running in Auto mode. If the machine is set to straight CPAP (or straight BiPAP), the machine will NOT record VS snores. If the machine is a model number 450/460 (System One PRO) or 650/660 (System One BiPAP PRO), the machine will NOT record VS snores.
The VS snores have time stamps attached to them, but they do not have a "magnitude" number. In the SleepyHead "events" list, when you look at the detailed information for each VS snore event, the number in parenthesis will always be a 0. But VS snores are the snores that cause the Auto algorithm to respond by increasing the pressure. (On a BiPAP Auto, it's the EPAP that is increased.) For each VS scored, the machine typically increases the pressure by 1 cm. Hence if there's a cluster of VS's, the machine will keep increasing the pressure until either the snoring stops or the max pressure setting is reached. It's also worth noting that in all the data we've seen, in dense clusters of VS snores, the VS snores appear to be scored in roughly one minute intervals---in other words, there is usually a full minute between adjacent VS snores.
In Encore, the VS's do NOT seem to show up as tick marks in the Events table. But it's hard to say for sure. Where they do show up is on the wave form when you look at it in Encore Pro (or EncoreBasic). Of course, Encore only downloads the wave form for the last night (or sometimes the last two nights) when you down load the data. Encore Pro at least stores all the previously downloaded wave forms in the patient's database, but EncoreBasic only stores the last wave form. SleepyHead also puts tick marks for VS snores on the wave form data when a Philips Respironics machine is running in Auto and the VS data is being recorded.
So as far as we can tell: The VS snores make up the part of the snoring data that is used by the Auto-algorithm when it determines that the snoring is significant enough to warrant an pressure increase. But no one (except the Philips Respironics engineers) know what the scoring criteria for a VS snore actually is.
VS2 snores
VS2 snores are recorded by all Philips Respironics machines. They have both a time stamp and a "magnitude" number attached to them. In the SleepyHead list, when you look at the detailed information for each VS snore event, there will be a NON-zero number in the in parenthesis for that event. Whether that number represents the length the snoring went on or some kind of measure of the loudness of the snoring is anybody's guess. We really do not know the significance of that number.
The SleepyHead VS2 graph uses the "magnitude" numbers for the vertical-coordinates in the Snore graph. In other words, the SleepyHead VS2 graph was set up with the assumption that the "magnitude" numbers are somehow related to how bad the snoring is. That's not a totally unreasonable assumption since you can have VS2 events closely space together with some rather large "magnitude" numbers. But it is an assumption and there's no real way to verify whether this assumption is valid. That's why the units on the Snore graphs are labelled as "Unknown" when you hover the mouse over the vertical scale of the Snore graph.
The VS2 snores show up in Encore (all versions) as tick marks in the Events table based on the time stamp of the VS2 event. But the calculation of the VSI index in Encore is not as straightforward as you would expect.
No one outside of Philips Respironics really knows the difference between the changes in flow rate that are needed to score a VS and the changes needed to score a VS2. But some of the Philips Respironics System One machines can be pretty sensitive to picking up vibrations that are coming from sources other than the patient's own airflow. But that said, real snoring is picked up by the Philips Respironics System One as well as false snoring. You basically have to look at patterns in your own data and learn to interpret based on what you know is going on at night and what you think might be going on at night.
The Snore Indices in SleepyHead and Encore
SleepyHead 0.9.6 calculates the VSnore Index shown in the left sidebar of the Daily Details data as follows:
- SleepyHead VSnore Index = (# of VS2 scored during the night)/(run time for the night)
And so the SleepyHead VSnore Index is nothing more than the average number of VS2 snores detected in an hour of sleep (or more technically run time).
Note: The VS events are not used to compute this index. This is important because:
- If you are using a Philips Respironics System One AUTO or BiPAP AUTO in FIXED pressure mode, your SleepyHead VSnore index will NOT include the VS snores in the Snore index.
Important Note for users of earlier versions of SleepyHead
In pre-0.9.5 versions of SleepyHead, the SleepyHead VSI index used VS snores to compute the VSI. If you are using a Philips Respironics machine in fixed pressure mode and SleepyHead 0.9.3 (or earlier), SleepyHead will report a VSI = 0.0 even if you are snoring your head off!
Snoring Data in Encore, (the official software for Philips Respironics machines)
Encore calculates the VSI shown on the right sidebar of the Encore Daily Detailed data in a really bizarre way. We can illustrate this with data from our sample patient's data. On July 31, 2013, she had 3 VS 2 snores scored for the entire night. In SleepyHead, the data looks like this:
- Vibratory Snore #2 3 events
- #001: 06:43:58 (2)
- #002: 06:54:13 (3)
- #003: 08:27:51 (1)
- Vibratory Snore 1 event
- #001: 06:53:41 (0)
Total run time for the night was 5:31:47, which is 5.53 hours. In Encore, the VSI on the right side of the Daily Detailed Data panel is reported as VSI = 1.1. Now Encore only shows three snore tick marks in the Events table on the daily data---one for each of the VS 2 snores. And the Encore Pro wave form shows only one snore tick mark---the one for the VS snore. So the total number of (relevant) snores is either 3 or 4 depending on whether the VSI is computed using just the VS 2's in the Event table or both the VS 2's and the VS snores shown only in the wave form.
But it's obvious that 3/5.53 is NOT equal to 1.1 and 4/5.53 is NOT equal to 1.1. Hence Encore is not computing its VSI by simply dividing the number of VS2 snores recorded during the night by the time the machine was running. Nor is it dividing the total number of snores recorded during the night by the time the machine was running.
Instead, with a bit of mathematical reverse-engineering, we can figure out that Encore computes the Encore VSI for the night as follows:
- Encore VSI = 1.1 = 6/5.53 - (2 + 3 + 1)/5.53 = (Sum of the "magnitude" numbers of the VS #2)/(run time)
And we've checked this "formula" out on many other nights-- some with rather large numbers of snores and some with small numbers. It always seems to be the case that:
- Encore VSI = (Sum of the "magnitude" numbers for the VS 2's as shown in SleepyHead)/(run time for the night)
Why would Encore define the VSI (Vibratory Snore Index) in this way? We have no idea. Mathematically it makes no sense. If the snores are being scored as "discrete" events (the same way the Flow Limitations are scored as "discrete events") then the intuitive meaning of VSI would be the average number of events per hour, and VSI ought to be (number of snores)/(run time)
So that then leads to the following speculation: Is it possible that the "magnitude" number on the VS2 snores represents something other than loudness (severity) of the snoring? Perhaps the "magnitude number represents the length of time measured in (seconds? minutes? number of breaths?) that snoring was being detected? In that case, the Encore VSI would then represent the average amount of "snoring time" in each hour of sleep measured in (seconds? minutes? number of breaths?)
Flow Limitations
For more information please see: Flow Limitation/UARS and BiPAP and Flow Limitation
Sleepyhead Flow Limitation
DeVilbiss machines do NOT record FL data; Fisher & Paykel Icons do record FL data Resmed graphs flow limitations on a scale of 0 to 1 Philips flags flow limitations as events.
Examples of respiratory wave form abnormalities including Flow Limitation
Sleepyhead Flow Limitation Example (Resmed)
In Sleepyhead, flow limitation is usually seen as a flattened inspiratory peak in the Flow Rate chart instead of the normal rounded wave-form. The following images show a moderate to severe flow limitation, and the same patient using EPR to achieve a normal inspiratory flow.
Fancy Stuff: Other Data Available from SleepyHead
UNDER CONSTRUCTION
TV, MV, and others. Also stuff for ASV users---Patient Triggered breaths, mask pressure etc. Also any other machine specific data: PB on ResMeds; SensAwake stuff for Icons; Expiratory Puffs (for either Icons or IntelliPAPs)
This is UNDER CONSTRUCTION and a very, very rough first draft of the material that will eventually be here.
Minute Ventilation is the total amount of air you breath in (or breath out) over the course of one minute. Unless you have a chronic daytime breathing problem like asthma or COPD, you can assume that these numbers are ok. They vary from person to person (based on size) and during solid sleep they are typically lower than when you're awake. Most don't tend to look at these numbers much, except as a curiosity.
Respiratory Rate.
These are the numbers for your respiratory rate-- i.e. how many times you breathe each minute. Again, they're going to vary from person to person. We're not sure why the min is so low here; it may be that during some part of the night there were some long apneas or several apneas close enough together to bring this down. If you've got copies of your sleep test you can compare the W-Avg, median, and 95% numbers to the respiratory rate on the sleep test if you want. Again, RR varies from person to person. For many people the RR goes down somewhat in solid sleep; for others it goes up.
Some people claim they can use the information from the RR graph and the minute ventilation graph or the tidal volume graph to distinguish possible REM cycles and possible arousals. Some are sceptical of such claims and don't think that we can pinpoint such things in our own data from these graphs.
Inspiratory:Expiratory (ratio)
Philips Respironics machines do not display this. Mathematically these numbers seem to be the Inspiratory Time in seconds divided by the Expiratory time in seconds, but perhaps this is actually being reported as a "percent" In other words, these numbers may actually be computed as:
- [(Inspiratory Time in seconds)/(expiratory Time in seconds)] * 100%
[Wiki Editor note: FIX THIS IT MAKES NO SENSE OUT OF CONTEXT OF THE ORIGINAL POST THIS WAS PULLED FROM] And in that case the meaning of the weighted average is that the length of your average inhalation is about 40% of the length of your average exhalation. In other words, the fact that all of these numbers are less than 100 means that your inhalations are shorter than your exhalations.
We have no idea if there is any clinical significance to this number or not. For most of us, it's likely not a very useful number to worry about.
Insp Time Inspiratory Time (seconds)
These are the numbers for the lengths of your individual inhalations. Is there any clinical significance to the length of the inhalations? Not that we know of-- if you don't have some kind of a daytime breathing problem as well as sleep apnea.
Exp Time Expiratory Time (seconds)
These are the numbers for the lengths of your individual exhalations. Is there any clinical significance to the length of the exhalations? Not that we know of-- if you don't have some kind of a daytime breathing problem as well as sleep apnea
Tidal Volume Tidal Volume (mL)
Tidal volume(symbol VT or TV) is the lung volume representing the normal volume of air displaced between normal inhalation and exhalation when extra effort is not applied. In a healthy, young human adult, tidal volume is approximately 500 mL per inspiration or 7 mL/kg of body mass.
Tidal volume is how much air you breath in during one inhalation. It's measured in mL and there are 1000 mL in one L. That's why these numbers are so much "bigger" looking than the minute ventilation numbers, which are measured in L/min.
The Tidal volume and the Minute Ventilation are related to each other:
- Minute Ventilation in L/min = (Tidal volume in mL/1000) * (Respiratory rate in breaths per minute)
Tidal volume is of great importance for people who are using an ASV machine since Tidal Volumes are used by the machine to figure out when to trigger inhalations. But for the rest of us? Tidal volume doesn't really have much significance if we don't have a daytime breathing problem.
Like Minute Ventilation and RR, the Tidal volume varies from person to person. And when we're asleep, our tidal volume typically is less than when we're awake. For now you can pretty much ignore the Tidal volume numbers.
Manipulating Daily and Overview Graphs
UNDER CONSTRUCTION
moving graphs around, turning graphs off, changing the scale of graphs
Tricks to remember to include:
Double clicking the Text label on an unpinned graph "pins" it to the top of the list of graphs. Double clicking the Text of a pinned graph unpins the graph and you can once again move it around.
The Event table is pinned by default. Double clicking on it will unpin it as well.
1) Zooming and unzooming. You can zoom in on the center of any of the Daily graphs by LEFT clicking when the mouse is over the graph. You can zoom back out by RIGHT clicking when the mouse is over the graph.
2) Scrolling through a Daily graph. Regardless of how far you have zoomed in on the graph, you can scroll through the graph by holding the RIGHT mouse button down while moving the mouse in a horizontal direction.
3) If Link Graph Groups is checked in the SleepyHead View menu, zooming in on one daily graph will cause all the daily graphs except for the Event table to zoom in by the exact same amount.
4) Glitches Sometimes you run into a SleepyHead glitch and the y-axis for the Flow Rate graph is off: The middle part of the breathing cycle is not graphed at 0 L/min. It's a known problem. If this happens to you, the easiest thing to do is just to mentally draw the 0.0 L/min line half way between the peaks and valleys in the Flow Rate graph and use that to measure when you are inhaling and exhaling.
And also add all the keyboard and mouse short-cuts and tricks:
- Holding in Control (or Command on Mac) and using the mouse wheel zooms in/out..
- Cursor up & down keys also zooms when the graph area has input focus.
- Cursor left and right keys scrolls the highlighted box.
- Holding in Control (or Command..) while left/right click zooming will cause it to zoom faster.
- Right clicking on, and then dragging the currently selected highlight in the event flags graph allows you to easily slide the current selected time "window" over the whole period.
- Right clicking on, and dragging any other graph will act as if you are picking it up and panning it left or right.
- Double clicking on the Y-Axis labels will toggle between auto-zoom and default zoom, provided it hasn't been overridden in graph preferences.
- Double clicking on the graph title text area pins or unpins any graph, so it remains always visible on screen, up the top. Your graph pins are persistent.
- Clicking on graph title text and dragging allows you to reorder the graphs (but pins will always be on top... Pins can be reordered amongst themselves too)
- Clicking on the date panel above the calendar widget toggles the calendar on/off to quickly give you more Details room in the left Daily panel.
- F8 key quickly toggles the right navigation panel to give you more graph room.
- You can drag the vertical sizer line that is between the left panel and graph area all the way to the left, allowing you to get full screen graphs.
- If you want to quickly view a single Daily graph full screen, hide the navigation panel and left panel as shown above, then minimise all graphs with the down arrow button next to the right side drop down in the bottom panel, then turn back on the graph you want in the drop down.
- To get all graphs visible again, click the arrows next to that combo box twice.
- Clicking on the grey line between graphs allows you to resize that particular graph. It will remember the graph heights for next time.
- The "Reset" button down the bottom panel of the graph area restores all graphs to uniform sizing.
- The "100%" button zooms out completely to show the entire day.
- You can click on the coloured event names in the Daily Details panel to jump to them highlighted in the Events tab
- You can click on the duration shown in the CPAP Sessions to highlight just that session.
- Clicking on the an entry in the Prescription changes list will jump to Overview and select that date range.
There is an option in Appearance preferences to dampen the horizontal left and right panning on sensitive Mac trackpads/mice... it allows you to define a millisecond delay between vertical scrolling and horizontal panning (without this setting, scrolling is a nightmare to use for people with shaky hands (like me)) on sensitive input devices. If you have trouble seeing the graph lines, you can now set the thickness of line plots in Appearance preferences.
(non bargraph) Overview graphs can be alternatively displayed as Line plots in Appearance preferences, which seem to be more attractive.
Tooltip durations can be altered in preferences... if you find them annoying drag it all or most of the way to the left.
Posting SleepyHead Graphs to the Forum
The overall process of posting an image of your data to the forum is pretty straight forward. You must:
- Decide what data you want to post.
- Create screenshots of the data you want to post.
- Upload the screenshots to a photosharing site OR a publically accessible Dropbox folder or GoogleDocs folder.
- Insert an image link in your post that points to the uploaded screenshot so that your image appears as part of your post. Each step of this process is examined below.
Decide what data you want to post
The data you want to post largely depends on what kind of feedback you want from the forum. You have to give us the data that is directly related to answering your questions. Many newcomers post random bits of data, only to be told that "We need to see X or Y instead (or in addition) to what you've shown us." So it helps everyone if you take the time to think about what data is needed to answer your questions.
Equipment description
Make sure your equipment profile is up to date and correct. Be precise in describing your CPAP equipment. There are six commonly used ResMed S9s and at least that many commonly used Philips Respironics System Ones; we need to exactly which model you are using. If you are including leak data, it helps to remind folks if you are using a FFM or not: It's irksome to be repeatedly told that you really need to switch to a FFM because of mouth breathing if you already use a FFM because you already know you're a mouth breather.
Getting feedback on the question: How am I doing?
If you are just wondering whether your data looks good, bad, or indifferent, it's useful to include the following things in your post:
- A screenshot of the following Overview Graphs
- AHI
- Usage (and Session Times if Sleep Fragmentation or Insomnia may be an issue)
- Leaks or Total Leaks (you don't need both; if you are using a NON-ResMed machine Total Leaks may be more useful)
- Peak AHI (particularly useful if you tend to have large clusters of events)
Be sure to choose an appropriate time frame for the Overview data. If you are wondering about just the last month, don't include a year's worth of Overview Data; similarly if you are wondering about the last three months, don't include just a week's worth of data.
- Screenshots of one or more typical night's Detailed Data. The screenshots should include the following:
- * The AHI table and the Statistical Data from the Left Side Bar.
- * The following Daily Graphs showing the whole night:
- * Event Flags
- * Flow Rate
- * Pressure (not really needed if you use fixed pressure and no ramp)
- * Leak
The Event Flags, Pressure, and Leak graph can usually be compressed vertically so these four graphs fit nicely on the screen. If you hide the Calendar and turn the Pie Chart off in the Left Sidebar of the Daily Data, you can show all the needed Daily Data in one screen shot.
Before you make your screen shots, it helps to:
- Hide the Right Sidebar. It adds no useful information.
- Hide the Calendar and turn the Pie Chart off in the Left Sidebar of the Daily Data.
- Adjust the size, scale, and order of the graphs you want to post. Hide all the unwanted graphs.
- Try to limit the number of graphs in each screen shot. When you try to cram more than five graphs into one screen shot, the graphs are so tiny they're hard to read.
Here's a useful screenshot of three months of Overview Data:
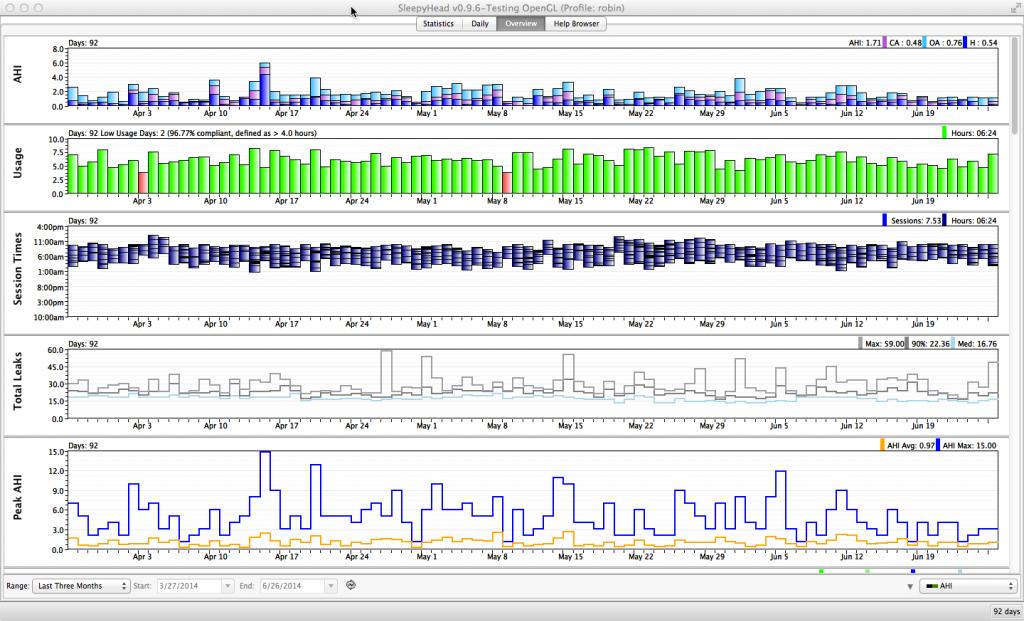
And here's a useful screenshot of the most important Daily Detail Data:
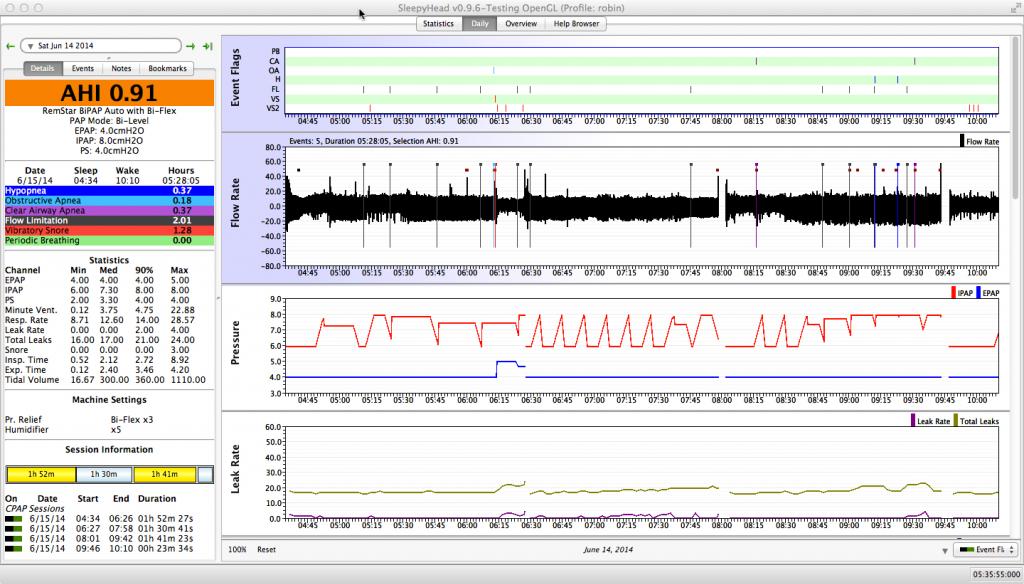
Getting feed back on specific questions or issues about what your data means
You need to include the right data at the appropriate level of magnification in order to get useful feedback to specific questions.
For example, if you are wondering what triggered a particular pressure increase, you need to zoom in on the Flow Rate, Pressure, Snore, and Flow Limitation graphs because the answer will lie in one of those graphs.
If you are concerned about clusters of events, it helps to provide a picture of the whole night's flow wave, a close up showing the flow wave for the cluster, and (perhaps) a close up that shows a few of the events at a scale where the individual breaths can be seen. If you are wondering whether the clusters indicate that you need to change the min/max pressure settings on your APAP, you need to include the Pressure graph as well as the Flow Rate.
If you are worried about leaks, it's useful to include the Flow Rate and Pressure graphs along with the Leak graph. Again both a global picture of the whole night and a close up of the troublesome leak (or a typical troublesome leak) will provide us with more information. And the more information we have, the better we can respond to your questions.
If someone asks you for additional data, it's useful to create another screenshot showing all the data---both the previously posted data and the requested data---rather than just a screen shot of the new graph.
In general when you are posting zoomed in Daily Data graphs, it helps to include the Events Table as well as the zoomed in graphs. That allows readers to put the posted data into the context of the full night.
Create screenshots of the data you want to post
If you already know a way of creating screenshots on your computer, just use what you already use. Be sure to save the screen shot as a .jpg, .jpeg, or .png file.
SleepyHead 0.9.6's built-in screenshot tool
SleepyHead 0.9.6 has a built-in screenshot tool that works well for most Macs and PCs. Once you have the window set up the way you want it to appear, simply press the F12 function key and SleepyHead 0.9.6 will a screen shot of the SleepyHead window. The screenshot will be saved in the SleepyHeadData/Screenshots folder. Unless you specify a different location for this folder, the SleepyHeadData folder is usually found in your Documents or My Documents folder. The naming convention for the screenshots is screenshot-yyyymmdd-hhmmss.png where yyyymmdd-hhmmss is the time the screenshot was taken. The hh part of the timestamp is in 24-hour format, so screenshot-20140628-183106 was taken at 6:31:06 pm on June 28, 2014.
I am told that the F12 trick will work for SleepyHead 0.9.3 screenshots on Windows machines. But if you are using SleepyHead 0.9.3 on a Mac, the F12 Sleepyhead screenshot shortcut will not work; however, you can use the standard cryptic Apple keyboard sequence to take the screenshot.
If you have any trouble with SleepyHead's built-in screenshot tool, you can always make the screenshots you need with the standard screenshot tools for your computer's operating system.
Macintosh Screen Shots
Press the Cmd, Shift, and 4 keys simultaneously, then hit the Space bar and then Left Click on the window you want the screen shot of; the screenshot will appear on your desktop with a file name like Screen Shot 2014-06-29 at 12.08.04 PM.png.
If you want to take a screen shot of only part of the SleepyHead window, press Cmd, Shift, and 4 keys simultaneously, and then use the mouse to select the part of the screen you want to capture. The screenshot will appear on your desktop. (Apple's instructions for screenshots can be found at http://support.apple.com/kb/ht5775 )
Windows Screen Shots
Instructions on how to make screenshots in Windows can be found at numerous sites on the web. These instructions from http://windows.microsoft.com/en-us/windows-xp/help/setup/take-a-screen-shot work on a Windows 7 computer.
To take a screenshot of the active window:
- Make sure the window is at the front and not covered by other windows,
- Press the Alt and PrtSc keys at the same time to copy the contents of the active window to the clipboard, and
- Paste the clipboard contents into a blank Paint document and save the image a .png (or .jpg) file.
If you want to take a screen shoto of only part of the SleepyHead window, you will need to use the MS Snipping Tool. You will need to:
- Open the Snipping Tool and select the kind of Snip (rectangular is the best choice),
- Use the mouse to capture the snip (it should appear in the Snipping Tool window), and
- Save the snip from inside the Snipping Tool window.
Complete instructions on how to use the Snipping Tool to create a screenshot of part of a window can be found at http://windows.microsoft.com/en-us/windows/use-snipping-tool-capture-screen-shots#1TC=windows-8
Insert the Screenshots into your forum posts
Once you have the images uploaded to a publicly accessible site on the web, you still need to properly insert a link into your post so that the image shows up inside the post. In order to make the link you need the web address (url) of the image. You can easily get that off of Photobucket or Flickr when you are looking at the image.
When you are writing a post and you reach the point where you want the image to appear, you need to copy and paste the url for the image into the post and then surround the url with the tags [img] and [/img] The tags [IMG] and [/IMG] will also work.
An example
So let's suppose that you want to put an image with the url:
http://i1198.photobucket.com/albums/aa456/robysue/Weird%20Wave%20Forms/001-07-15-OA-do-you-see-one.jpg into your post. You need to write this inside the editing window for the post:
- ... So what's going with this oddball part of the Flow Rate?
- ... So what's going with this oddball part of the Flow Rate?
- [img]http://i1198.photobucket.com/albums/aa456/robysue/Weird%20Wave%20Forms/001-07-15-OA-do-you-see-one.jpg[/img]
- [img]http://i1198.photobucket.com/albums/aa456/robysue/Weird%20Wave%20Forms/001-07-15-OA-do-you-see-one.jpg[/img]
- Did the machine just plain make a mistake and score an apnea where there wasn't one?
in order to make the post look like this:
... So what's going with this oddball part of the Flow Rate?
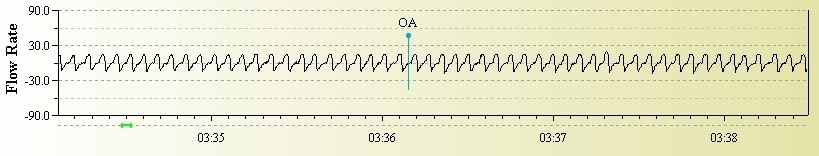
Did the machine just plain make a mistake and score an apnea where there wasn't one?
Special Notes
If you use Photobucket, you can simply copy and paste the IMG link into the editing window for the post. The Photobucket link will automatically include the [IMG] and [/IMG] tags as well as a URL link.
On the Apnea Board forums, the "Insert Image" button looks like a sun over some mountain peaks and it brings up a pop-up box that looks like this:
To insert the image, simply past the url into the pop-up box and click Okay or hit enter. You'll get something like this:
- [img]http://i1198.photobucket.com/albums/aa456/robysue/Weird%20Wave%20Forms/001-07-15-OA-do-you-see-one.jpg[/img]
inside the edit window for the post.
For more information about posting links to image files on the Apnea Board forum, see the post Inserting an Image in the Member Account Help Forum in the private area of the Apnea Board forums (free registration required for access).
Tricks and Shortcuts
These are tricks and shortcuts that work in SleepyHead. Some of them manipulate graphs, others help your navigate around SleepyHead quickly.
Note: Tricks and shortcuts appear on this list more than once because we think of them in more than one way.
Tricks for moving around SleepyHead and changing the appearance of the SleepyHead windows
- Cursor left and right keys scrolls the highlighted box. If the calendar is highlighted, these keys will move the Daily Detailed data backward or forward by one day at a time.
- Right clicking on, and then dragging the currently selected highlight in the Event Table allows you to easily slide the current selected time "window" over the whole period.
- Right clicking on, and dragging any graph other than the Events Table will act as if you are picking it up and panning it left or right.
- Double clicking on a graph's title text area pins or unpins any graph. Pinned graphs always remain visible on screen, up the top. Your graph pins are persistent.
- Clicking on graph title text and dragging allows you to reorder the graphs, but pinned graphs will always be on top. Pinned graphs can be reordered amongst themselves in this same way.
- Clicking on the date panel above the Daily Detail calendar toggles the calendar on/off to quickly give you more room in the Left Sidebar of the Daily Data for the statistical data
- F8 key quickly toggles the right navigation panel to give you more graph room.
- You can drag the vertical sizer line that is between the left panel and graph area all the way to the left, allowing you to get full screen graphs.
- If you want to view only ONE of the Daily graphs or ONE of the Overview graphs, you can minimize all the graphs with the down arrow button next to the right side drop down in the bottom panel, then turn back on the graph you want to look at in the drop down menu in the bottom left corner. To make all the graphs visible again, click the arrows next to that drop down menu box twice.
- The "Reset" button down the bottom panel of the graph area restores all graphs to uniform sizing.
- You can click on the colored event names in the Daily Details panel to jump to them highlighted in the Events tab
- You can click on the duration shown in the CPAP Sessions to highlight just that session.
- Clicking on the an entry in the Prescription Changes list in the Statistics page will jump to Overview and select that date range.
- Tooltip durations can be altered in the Appearance Preferences. If you find them annoying drag it all or most of the way to the left.
- Shift-click on a date in the Overview screen and SleepyHead takes you to that date in Daily Data view.
Tricks and shortcuts to manipulate graphs
- Holding in Control (or Command on Mac) and using the mouse wheel zooms graphs in/out
- Cursor up & down keys zooms when the graph area has input focus.
- Cursor left and right keys scrolls the highlighted box. If the Daily Data or Overview graphs are highlighted, this will provide a horizontal scroll.
- Holding in Control (or Command..) while left/right click on a graph will cause it to zoom faster.
- Right clicking on, and then dragging the currently selected highlight in the Event Table allows you to easily slide the current selected time "window" over the whole period.
- Right clicking on, and dragging any graph other than the Events Table will act as if you are picking it up and panning it left or right.
- Double clicking on the y-axis labels will toggle between auto-zoom and default zoom, provided the graph's y-range hasn't been specified in the Graph Preferences
- Double clicking on a graph's title text area pins or unpins any graph. Pinned graphs always remain visible on screen, up the top. Your graph pins are persistent.
- Clicking on graph title text and dragging allows you to reorder the graphs, but pinned graphs will always be on top. Pinned graphs can be reordered amongst themselves in this same way.
- You can drag the vertical sizer line that is between the left panel and graph area all the way to the left, allowing you to get full screen graphs.
- Clicking on the grey line between graphs allows you to resize that particular graph. SleepyHead will remember the graph heights for next time.
- If you want to view only ONE of the Daily graphs or ONE of the Overview graphs, you can minimize all the graphs with the down arrow button next to the right side drop down in the bottom panel, then turn back on the graph you want to look at in the drop down menu in the bottom left corner. To make all the graphs visible again, click the arrows next to that drop down menu box twice.
- The "Reset" button down the bottom panel of the graph area restores all graphs to uniform sizing.
- The "100%" button zooms out completely to show the entire day.
- You can click on the duration shown in the CPAP Sessions to highlight just that session.
- If you have trouble seeing the graph lines, you can now set the thickness of line plots in Appearance Preferences
- Overview graphs can be alternatively displayed as Line plots (non-bar graphs) in Appearance Preferences
Keyboard tricks and shortcuts
- Cursor up & down keys zooms when the graph area has input focus.
- Cursor left and right keys scrolls the highlighted box. If the graphs are highlighted, this will provide a horizontal scroll; if the calendar is highlighted, these keys will move the day data backward or forward by one day at a time.
- F8 key quickly toggles the right navigation panel to give you more graph room.
- F11 key quickly toggles to and from Full Screen view.
- F12 key takes a screenshot of the current SleepyHead window; the screenshot will be saved to your SleepyHeadData/Screenshots folder.
Useful tricks with the mouse
- Holding in Control (or Command on Mac) and using the mouse wheel zooms graphs in/out
- Holding in Control (or Command..) while left/right click on a graph will cause it to zoom faster.
- Right clicking on, and then dragging the currently selected highlight in the Event Table allows you to easily slide the current selected time "window" over the whole period.
- Right clicking on, and dragging any graph other than the Events Table will act as if you are picking it up and panning it left or right.
- Double clicking on the y-axis labels will toggle between auto-zoom and default zoom, provided the graph's y-range hasn't been specified in the Graph Preferences
- Double clicking on a graph's title text area pins or unpins any graph. Pinned graphs always remain visible on screen, up the top. Your graph pins are persistent.
- Clicking on graph title text and dragging allows you to reorder the graphs, but pinned graphs will always be on top. Pinned graphs can be reordered amongst themselves in this same way.
- Clicking on the date panel above the Daily Detail calendar toggles the calendar on/off to quickly give you more room in the Left Sidebar of the Daily Data for the statistical data
- You can drag the vertical sizer line that is between the left panel and graph area all the way to the left, allowing you to get full screen graphs.
- Clicking on the grey line between graphs allows you to resize that particular graph. SleepyHead will remember the graph heights for next time.
- You can click on the colored event names in the Daily Details panel to jump to them highlighted in the Events tab
- You can click on the duration shown in the CPAP Sessions to highlight just that session.
- Shift-click on a date in the Overview screen and SleepyHead takes you to that date in Daily Data view.
- There is an option in Appearance Preferences to dampen the horizontal left and right panning on sensitive Mac trackpads/mice. This allows you to define a millisecond delay between vertical scrolling and horizontal panning. Without this setting, scrolling is a nightmare to use for people with shaky hands on sensitive input devices.
SleepyHead FAQ
Q: Can SleepyHead change or erase the data on my SD card?
A: No. SleepyHead only reads the data on the SD card; it never writes anything to the SD card. Note, however, that some computer operating systems may write hidden files to the SD card. So it is a good idea to lock the SD card before you put it into your computer's SD card slot.
Q: I imported my data into SleepyHead and when I put the card back into my ResMed S9, I get an error that says: " 'Invalid SD card, erase card data?". Why is this happening and what should I do?
A: SleepyHead did not cause the problem; your operating system did. The operating system wrote some hidden files to the card, and the S9 does not want anything on the SD card that it did not write to the card. All versions of Mac OSX will write hidden files to an unlocked SD card. Windows 8.1 and Windows 10 are also known to write hidden files to an unlocked SD card. To fix the problem:
- Let the S9 erase the card and rewrite the summary and compliance data to the card. You will NOT lose any data that you've already imported into SleepyHead. And the summary and compliance data that your DME and sleep doc care about will be written back to the card.
- To prevent the problem in the future: Be sure to lock the SD card before inserting the SD card into your computer or card reader. You lock the SD card by sliding the "Lock" tab on the side of the card to the Locked position. That will prevent the operating system from writing hidden files to the SD card.
- After importing data into SleepyHead and removing the SD card from your computer, remember to unlock the card before putting it back into your S9 CPAP. If you forget to unlock the card, you might see an error message on the S9's LCD telling you that the inserted card is read only.
NOTE: Using ResScan on a Win 8.1 or Win 10 machine will NOT prevent this problem from happening; Windows will still write hidden files to an unlocked SD card and when you put the card back in the S9, the S9 will still insist on erasing the contents of the card.
NOTE AND WARNING for WIN 8.1 and Win 10 USERS
Some Win 8.1 & Win10 users have reported that locking the SD card does NOT prevent their computer from writing files to the SD card. The lock switch on the SD card is a physical switch and not all SD card readers have a corresponding physical switch in them that recognizes and respects the SD card's lock switch. You can test whether your Win 8.1 machine will ignore the Lock switch by doing the following:
- Step 1) Place a Locked SD card into the machine. I'd suggest an SD card that is NOT the one from your S9 machine.
- Step 2) Try to save a file of your choice to the SD card in the usual way.
If the computer writes the file to the SD card, then you know that the simple fix of locking the SD card is NOT going to work on your computer and its SD card slot: The Win 8.1 and Win 10 operating systems will continue to write those hidden system files to the SD card in spite of the card being locked.
What to do next depends on which Windows operating system you have and how comfortable you are with some advanced features of the operating system. Here are two things you can try:
- Try an external SD card reader plugged into a USB port. If the external SD card reader has the right kind of physical switch to detect the position of the SD card's lock tab, that should prevent Win 8.1 or Win 10 from writing the system files to the SD card.
- Try following these instructions from MS about how to prevent Windows from writing system files to removable media Note that these instructions specifically indicate that some of the suggestions are NOT applicable to Windows 8.1 Home edition.
Q: Will SleepyHead work on my computer?
A: SleepyHead will work on PCs running anything from Windows XP through Windows 10; it will also run on Macs running OS X 10.6 and later. SleepyHead 0.9.6 may have problems running on Windows XP, Windows Vista, and Mac OS X 10.6. Future versions of SleepyHead may not run on XP, Vista, or OS X 10.6. (NOTE: Windows XP and Mac OSX 10.6 have been completely left for dead by their creators, and users of these operating systems are running a great security risk if they use them online.) SleepyHead will also run on many flavors of Linux, but it is harder to install under Linux.
Q: My computer doesn't have an SD card slot. Can I still use SleepyHead?
A: Yes. You may use any generic SD card reader to access the data on the SD card. Generic SD card readers are readily available at office supply stores and big box stores like Target and Walmart. They usually cost less than $10 or $15.
Q: Is there a list of keyboard short cuts and mouse tricks for SleepyHead?
A: Yes. Go to 15. Tricks and Shortcuts
Q: I forgot to put my SD card back into my CPAP after importing the data into SleepyHead. Have I lost my data?
A: All modern CPAPs store the compliance data on-board and they will write that data to the SD card when the SD card is reinserted into the CPAP. Some CPAPs store a fair amount of other data on-board as well as the compliance data, and all of the on-board data will be written to the SD card. How much data you will see for the night in SleepyHead depends on both the brand of CPAP you use and the version of SleepyHead you use.
- Philips Respironics System One users will lose the Flow Rate data and the "fancy stuff" computed from the Flow Rate data. But the Event Table, Pressure graph, and Leak graph should all show up in the Daily Graphs along with the daily summary data in SleepyHead 0.9.3.
- ResMed S9 users will lose all of the detailed daily data and all of the Daily Data graphs. But summary data for the day should show up in SleepyHead 0.9.6.
- We don't know exactly what Fisher & Paykel Icon or DeVilbiss users will lose.
Q: How often do I need to import my data into SleepyHead?
A: It depends on the kind of CPAP you are using.
- ResMed S9 users need to import the data on a weekly basis if they want to see all available data, including the Flow Rate graph; the S9 overwrites the high resolution data (including the Flow Rate data) on a seven day cycle: In other words, tonight's high resolution data replaces the high resolution data from one week ago. The rest of the detailed daily data (pressure, leak, event table), is overwritten every 30 days.
- Fisher & Paykel Icon users need to import the data on a weekly basis; the Fisher & Paykel Icon overwrites the daily detailed data on a seven day cycle: In other words, tonight's detailed daily data replaces the high resolution data from one week ago.
- Philips Respironics System One and DeVilbiss IntelliPAP users can download much less frequently. These machines store several months to a year's worth of full efficacy data on the SD card. It's still not a bad idea to import the data into SleepyHead on regular basis in case the SD card becomes corrupted.
Q: I've downloaded my data from a ResMed S9 Elite, AutoSet, VPAP S, or VPAP Auto, and there is no detailed data and SleepyHead says I didn't use the machine. What did SleepyHead do with my data?
A: SleepyHead didn't do anything with your data. The most likely cause for your problem was that the card was left out of the S9 over night. (Or the card was not fully inserted.) If the SD card is not inserted into the S9 during the night, all the daily detailed data (including all the graphs) is lost; the S9 writes the detailed daily data directly to the SD card. The summary data, including the usage data, the overnight AHI, the overnight median, 95%, and maximum pressure levels, and the leak data overnight median, 95%, and maximum leak rate data, is stored in the S9's internal memory and is written back to the SD card when you re-insert the card. But SleepyHead cannot use this summary data for anything on the Daily Data page, and hence if you forget to put the SD card back into your machine, you won't get the graphs. Early versions of SleepyHead (including SleepyHead 0.9.3) cannot use the S9 summary data at all, and hence an early version of SleepyHead will tell you that there is no data for the day and "claim" that you did not use the machine. SleepyHead 0.6 should import the summary data into the Statistics page, although the calculated averages and percentiles using data from nights with no detailed daily data may not be mathematically accurate. The reason is that there's not enough data to accurately calculate the over night numbers if there are multiple sessions.
Q: I don't see any Flow Rate data. What am I doing wrong?
A: DeVilbiss IntelliPAP users will not see any Flow Rate data because the IntelliPAP does not record that data to the card. ResMed S9, Philips Respironics System One, and Fisher & Paykel Icon users will only see Flow Rate data if the card was in the machine while it was running; the Flow Rate data is written directly to the card. ResMed S9 and Icon users who do not down load their data at least once a week will only get the last 7 days of Flow Rate data for each down load: The S9 and the Icon both overwrite the Flow Rate data once a week.
Q: Can SleepyHead work with data from an oximeter?
A: Yes, SleepyHead can work with some O2 monitoring devices. See Importing CMS 50D Plus oximeter data into SleepyHead for details.
Q: Can SleepyHead tell me when I was in REM sleep?
A: No. Your CPAP does not record EEG data, which is needed to determine REM.
Q: Can SleepyHead tell me when I was awake during the night?
A: No. Your CPAP does not record EEG data, which is needed to determine night time wakes.
Q: Can SleepyHead tell me when I was sleeping on my back?
A: No. Your CPAP does not record positional data. SleepyHead can sync with Somnopose software
Q: I'd like to post some SleepyHead data to the forum, what should I do?
A: For tips and instructions on posting SleepyHead data to the form go to 14. Posting SleepyHead Graphs to the Forum
Q: Where can I report bugs?
A: If you are familiar with Sourceforge, you may report bugs on the SleepyHead project page. If you would rather not report the bug there, you may post the bug on Apnea Board's Software Support Forum. For a bug report to be useful, you need to include:
- The version of SleepyHead you are using
- Your operating system (be specific)
- Your computer's machine's make and model
- Your CPAP make and model
- A screenshot showing the bug
If you are reporting a bug that crashes SleepyHead, indicate what you were doing at the time of the crash.

Donate to Apnea Board