CPAP Data Interpretation
Contents
Introduction
- This article and associated pages discuss the interpretation of data created by CPAP machines (of all types) and viewed using suitable software. Although the principles are software-independent, for convenience we will base the discussion on OSCAR. However much of what is discussed in these pages will also apply to ResScan, Encore, Prisma TS and other apnea software.
- For details of the OSCAR program, see OSCAR Help.
- Acknowledgement: Much of the material in this help system has been taken and/or adapted from RobySue's Beginner's Guide to SleepyHead
Events – Apnea, Hypopnea etc
Event flag graph and events table
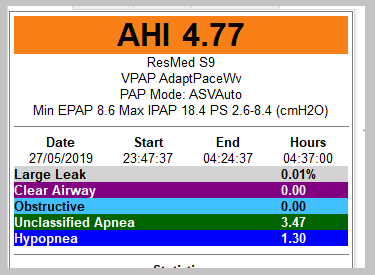
Events such as apneas, hypopneas, large leaks and other are shown in three ways in OSCAR:
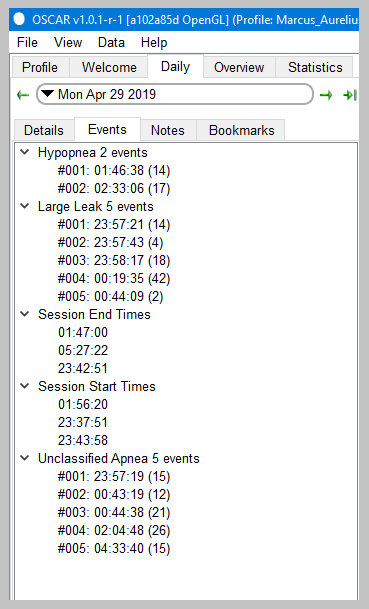
- The events table is accessed via the Events tab in the left side bar of the Daily page. It will list every occurrence of an apnea and other events, together with the time they occurred and the duration in seconds. The various sub-headings can be expanded. Click on any event to go to that same event in the graphs.
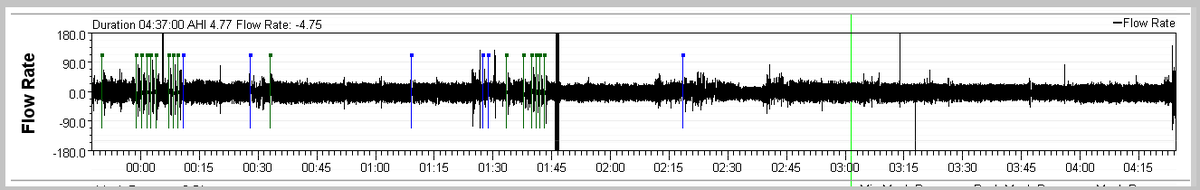
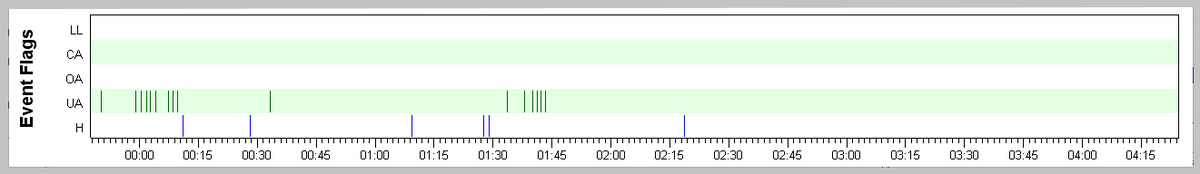
- The Events graph is normally the top-most graph on the Daily page, and shows each event as a vertical stroke. When zooming in on the other graphs, the Events graph will remain as is, with the zoomed in part of the night highlighted on the events graph. So it also provides a useful reference tool for being able to quickly put the zoomed in graphs into the context of the whole night.
- Events can also be shown on the Flow Rate graph and other graphs.
- The event index (ie number per hour) is shown in the left sidebar.
|
 |
The Event graph---a detailed look
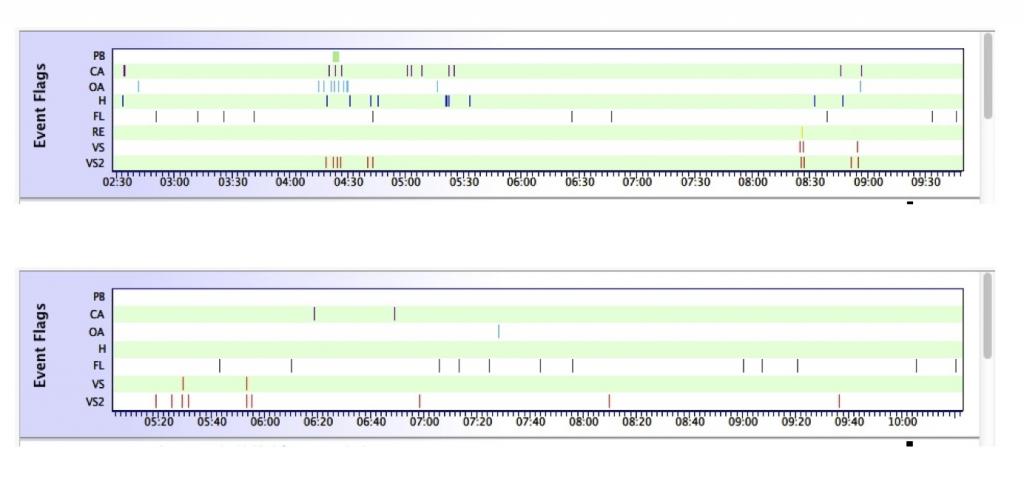
The Event graph gives a snapshot of how good or bad the whole night was, and whether certain parts of the night were much uglier than the overall AHI might indicate. Compare these two event charts:
You don't need the actual AHI numbers to see that the first night was a lot worse than the second. On the second night, there are only three "events" scored all night: Two CAs and one H. There are a few flow limitations, but even the FL are well spaced. And the bit of snoring at the beginning of the night is not a real issue. Overall, this night's efficacy data is really quite good.
But on the first night, there are a lot more tick marks over all AND between 4:15 and 5:30 there are a lot of OAs, Hs, and CAs scored. There's a second smaller cluster of events around 8:30 as well. The other thing we can immediately see about the first night is that outside of the 4:15-5:30 and 8:30-9:00 time frames, the rest of the night was pretty good.
The Event graph tells us where to look if we want (a lot) more information about periods with "bad night-time breathing." On the top night's data, it's worth zooming in on the 4:15-5:30 to see just how ugly things are. When we zoom in on the daily graphs, the Event graph remains fixed, but the zoomed in time frame is highlighted as shown:
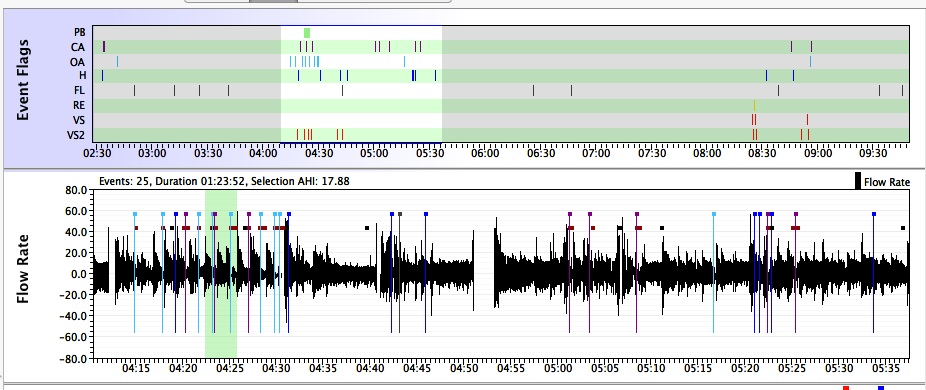
The highlighting on the Event graph gives a quick visual reference of where the zoomed in data comes from. That's useful if you start scrolling through zoomed in Flow Rate data for a whole night and notice something of interest. In other words, the Event Table serves as a "navigation" tool when you are looking at zoomed in detailed data.
When posting screen shots of zoomed in daily data, it is useful to include the Events graph in the screen shot so the others can get a sense of how the selected detailed data fits into the night as a whole.
Flow rate graph
Beyond AHI: Apneas and hypopneas in the flow rate graph
Beyond AHI: Apneas and hypopneas in the Flow Rate graph
Snoring
Flow limitations
Machine reaction to events
How APAP machines respond to events
New CPAP users are sometimes surprised by the fact that their CPAP did nothing when an apnea was in progress. There's an assumption that the positive air pressure provided by the CPAP is supposed to "blast" through the obstruction and restart the breathing. But pressure is not used to try to "end" an on-going event. It's not even clear that 20cmH20, the maximum pressure delivered by a CPAP, would even be effective at trying to "blow" a collapsed airway open: 20cmH20 is not enough pressure to effectively blow up an ordinary balloon. In fact, 20 cmH20 is about the difference in atmospheric pressure between a very stormy, low pressure day, and a bright sunny high pressure day.
The basic idea in CPAP therapy is to provide (a small bit of) positive air pressure through the entire breath cycle to make it more difficult for your airway to collapse. This system is very good at preventing apneas and hypopneas from occurring, but it is not perfect: A few events will likely occur each night, but the overall number of events will be low enough to keep your treated AHI under 5.0, and probably well under 5.0, each night you use the machine. In other words, a well-adjusted CPAP makes it difficult, but not impossible for your airway to collapse.
CPAPs, of course, cannot respond to OAs and Hs by increasing pressure since they have one fixed pressure setting. APAPs do respond to OAs and Hs, but it's important to realize that an APAP will wait until the apnea or hypopnea is over before it increases the pressure. And even then, a typical APAP won't raise the pressure after each and every OA or H. Rather, APAPs will only raise the pressure in response to OAs and Hs if two or more events occur in a relatively small amount of time like 5 minutes or so. The rationale for this behavior is based on the AASM Clinical Guidelines for Manual Titration Sleep Studies. Isolated OAs and Hs are not necessarily indicative of a badly compromised airway: Even normal people have the occasional (frank) OA or H during their sleep. But two or more OAs or Hs occurring close together indicates that the current pressure may not be sufficient to prevent the airway from collapsing in the (very near) future. And since more pressure is needed to prevent future events from happening, the machine increases the pressure after the second (or latest) event in the cluster ends.
APAPs also respond to snoring and flow limitations by increasing the pressure. Snoring and flow limitations are considered precursor events to OAs and Hs. In other words, snoring and flow limitations are thought to indicate that the airway is compromised: It may be partially collapsed (but not far enough to score an H) or it may be just barely beginning to collapse. More pressure at this point will help hold the airway open and prevent further collapse, and hence, prevent OAs and Hs from occurring. It's worth noting that some brands of APAPs are very aggressive in how fast and how far they increase pressure in response to snoring or flow limitations.
So the overall goal in every manufacturer's Auto-algorithm is to increase the pressure just enough to prevent more events from happening in next few minutes and allow the breathing to stabilize. The idea is to avoid jacking up the pressure unnecessarily: That can lead to more unstable breathing, discomfort, and more pressure than is needed to keep the airway open most of the time. And once the machine is satisfied the breathing is indeed stable, the Auto-algorithm will decrease the pressure until there is evidence that the airway is once again in some danger of collapsing.
Each manufacturer's Auto-algorithm handles the details of how to handle the pressure increases and decreases in its own proprietary way. Some machines are more aggressive and increase pressure faster in response to snoring, flow limitations, and events. Some take small 1cm steps in increasing the pressure and then wait for a minute or more before increasing the pressure further. The Philips Respironics machines even have a search algorithm that periodically tests what happens to the Flow Rate curve when a modest pressure increase is applied even when there are no scoreable events (OAs, Hs, FLs, RERAs, and Snoring). And likewise, each manufacturer's algorithm has a different way of deciding when to start decreasing the pressure and how fast to decrease the pressure.
It's clear from reading informational material aimed at clinicians, that each manufacturer believes that they have the "best" algorithm. But what little information that has been published about independent bench trials seems to indicate that while real differences in the auto-algorithms can be quantified, the clinical significance of those differences is much harder to evaluate. This may be one reason that some sleep docs are so reluctant to prescribe APAP therapy as the first course of treatment for ordinary OSA.
Pressure
Leaks
- OSCAR leaks
- Leak Rate Graph: A closer look
Other parameters

Donate to Apnea Board